
 English
English
 French
French
Impact of surgical treatment in acquired dipaphragmatic eventration: experience of a Moroccan center
Impact du traitement chirurgical dans l'évènementration dipaphragmatique acquise: expérience d'un centre Marocain
M. Massine El Hammoumi, M. Bhairis, A. Alassane, M. Amraoui, M. Kamdem, F. El Oueriachi, El H. Kabiri
Department of Thoracic Surgery, Mohamed V Military University Hospital, Rabat, Morocco
Faculty of Medicine and Pharmacy, Mohamed V University, Rabat, Morocco
Corresponding author
Dr. Mohammed Massine El Hammoumi
Department of Thoracic Surgery, Mohamed V Military University Hospital. Riad 10100, Rabat, Morocco.
E-mail: hamoumimassine@hotmail.fr
DOI: 10.12699/jfvpulm.12.36.2021.42
ABSTRACT
Background. Diaphragmatic eventration (DE) is defined as an abnormal elevation of the hemidiaphragm with abdominal structures migration. We report a retrospective study to emphasize the role of surgical repair.
Methods. From January 2006 to December 2018. In group A : 48 cases of asymptomatic DE weren’t operated and receive exclusive medical treatment by physical respiratory therapy. In group B: 38 symptomatic patients underwent plication surgery. The change in radiological eventration levels and in restrictive respiratory syndrome parameters (FEV1, FVC) of respiratory function tests performed during pre- and postoperative periods were compared in group B.
Results. The thoracic approach of DE can allow a real benefit as reported in the group B. The median duration of chest tube drainage was 2 days. In the same group of patients, 3 of them were complicated by hemothorax (n=2) and pyothorax (n=1) , a secondary surgery was mandatory. Clinical benefit of the surgery was objectified in 29 cases (78%) based on a satisfactory classical questionnaire. In the group A, only 11 patients (22.9%) reported an objective improvement after medical therapy (mainly functional rehabilitation). The difference between the two groups is statistically significant (p=0.025).
Conclusion. Diaphragmatic eventration is a rare condition, more frequently diagnosed on the left than on the right side. Surgical treatment have an objective impact on clinical function.
KEYWORDS: Eventration; Diaphragm; Surgery; Phrenic nerve; Palsy.
RÉSUMÉ
Introduction. L'événementration diaphragmatique (DE) est définie comme une élévation anormale de l'hémidiaphragme avec migration des structures abdominales. Nous rapportons une étude rétrospective pour souligner le rôle de la réparation chirurgicale.
Méthodes. De janvier 2006 à décembre 2018. Dans le groupe A: 48 cas de DE asymptomatique n'ont pas été opérés et bénéficient d'un traitement médical exclusif par kinésithérapie respiratoire. Dans le groupe B: 38 patients symptomatiques ont subi une chirurgie de plication. L'évolution des niveaux d'événements radiologiques et des paramètres restrictifs du syndrome respiratoire (FEV1, FVC) des tests de la fonction respiratoire effectués pendant les périodes pré et postopératoires a été comparée dans le groupe B.
Résultats. L'approche thoracique de l'ED peut permettre un réel bénéfice comme rapporté dans le groupe B. La durée médiane du drainage de la sonde thoracique était de 2 jours. Dans le même groupe de patients, 3 d'entre eux étaient compliqués d'hémothorax (n = 2) et de pyothorax (n = 1), une chirurgie secondaire était obligatoire. Le bénéfice clinique de la chirurgie a été objectivé dans 29 cas (78%) sur la base d'un questionnaire classique satisfaisant. Dans le groupe A, seuls 11 patients (22,9%) ont rapporté une amélioration objective après un traitement médical (principalement une rééducation fonctionnelle). La différence entre les deux groupes est statistiquement significative (p = 0,025).
Conclusion. L'événementration diaphragmatique est une affection rare, plus fréquemment diagnostiquée du côté gauche que du côté droit. Le traitement chirurgical a un impact objectif sur la fonction clinique.
MOTS CLÉS: Eventration; Diaphragme; Chirurgie; Nerf phrénique; Paralysie.
INTRODUCTION
Different from a diaphragmatic hernia, diaphragmatic eventration (DE) is Defined as an abnormal elevation ,without injury of the hemidiaphragm or part of it, with abdominal structures migration. More frequent in the pediatric population with congenital causes than in adults. The incidence is less than 0.05%.
The most common causes are prevous mediastinum surgery, chest trauma, neuromuscular diseases, some viral infection, and malignity. One-sided DE is rarely symptomatic in adults and the radiological diagnosis is the first diagnosing step. Dyspnea can be a common symptom. Respiratory distress can be described in bilateral DE. One of the hard steps in radiological diagnosis is rapid confusion with a diaphragmatic rupture particularly after thoraco-abdominal trauma situation or post-surgery.
Majority of reported studies of surgical treatment have raised discussions about indications of surgery on diaphragm eventration [1-5]. We report a retrospective study to emphasize the role of surgery in this condition within the scope of the existing literature.
METHODS
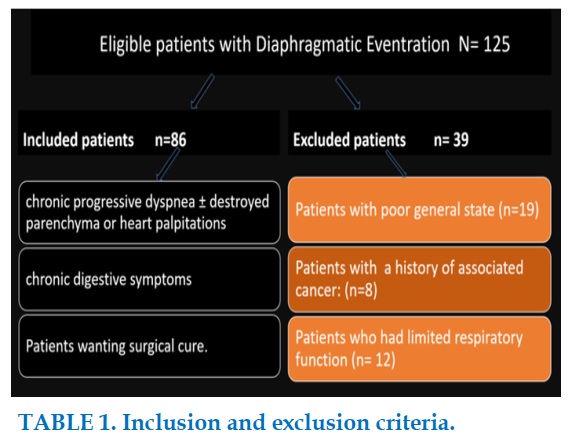
From January 2006 to December 2018, 125 cases of diaphragmatic eventration were treated in our unity. Thirty nine cases of them were excluded. Exclusion criteria of patients from our study are patients with poor general state, patients with a cancer, and patients with limited respiratory function (Table 1).
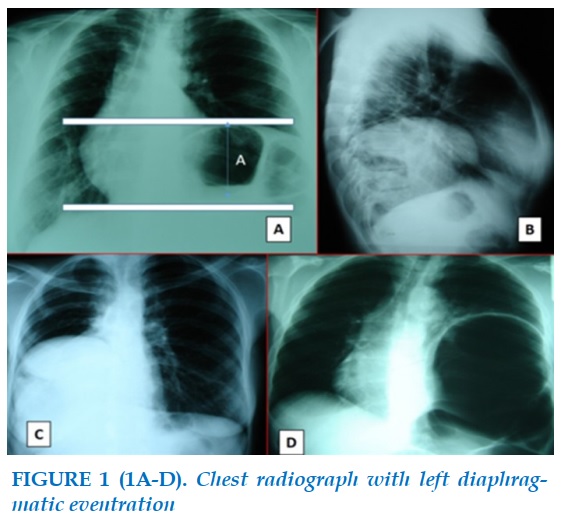
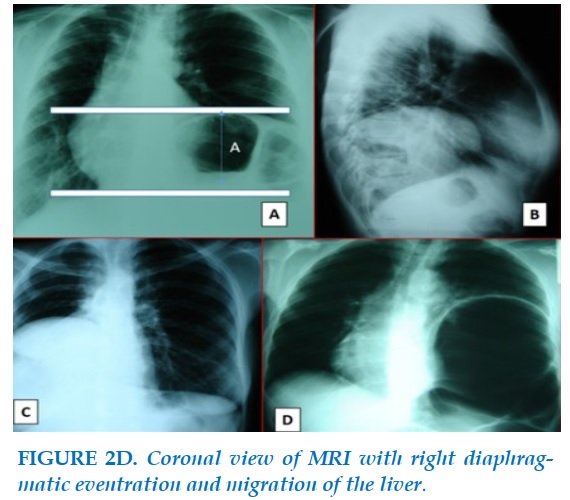
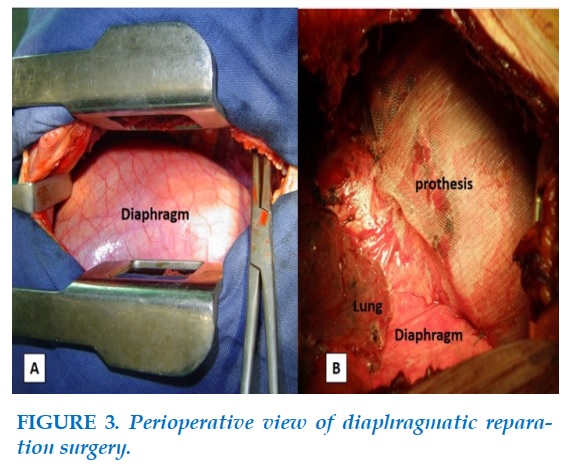
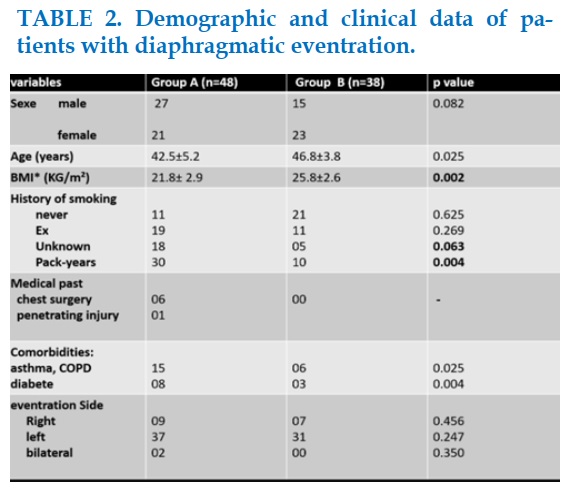
All patients underwent a chest radiograph and CT (Figure 1 and 2A-C), MRI was indicated in few cases (n=4) (Figure 2D). Respiratory functional tests were mandatory for all cases. The patients were divided into two groups based on initial diagnosis. In group A: 48 cases of asymptomatic DE weren’t operated and receive exclusive physical respiratory therapy. In group B: 38 symptomatic patients underwent plication surgery (Figure 3). Patient characteristics are presented in Table 2.
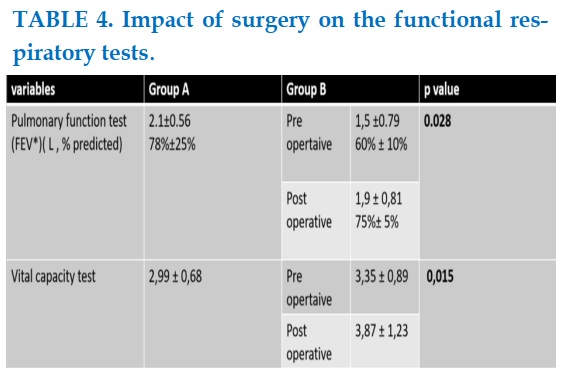
Respiratory function tests RFT (FEV1, FVC) were performed during pre- and postoperative periods (03 months later) and were compared only in group B. In this way, the effect levels of eventration changes on RFT were assessed.
Surgery
Surgical treatment of DE was indicated when patients had chronic progressive dyspnea or heart symptoms, chronic digestive symptoms or when patients desired surgical cure.
Operation procedures
General anesthesia with a double-lumen endotracheal tube to allow selective lung ventilation was prescribed for all operated patients. The patients were placed in the lateral decubitus position. Thoracoscopic approach was attempted in 03 cases and classical posterolateral thoracotomy in most cases. All operated cases underwent diaphragmatic plication surgery through a thoracotomy excepted in three cases, for which a minimally invasive technique was used. The mean argument to perform this classical approach is the delay of diagnosis that is often longer and patients develops serious pleural adhesions.
During thoracotomy, the seventh or eighth intercostal space was chosen to enter and diaphragmatic eventration was observed. We started the procedure on the central tedious part of the diaphragm using seven to nine lines of silk sutures from the posteromedial to anterolateral and by crossing the phrenic nerve fibers. Hanged sutures, and parallel plication were performed with central diaphragmatic repositioning. In some cases the use of reenforcing prosthetic plaques was necessary. In the end of surgery a 28-32Fr chest tube were inserted.
Postoperative chest tube management
A negative suction was applied immediately after operation and maintained until chest tube removal.
The chest tube was rapidly removed since this extrapulmonary surgical cure.
Statistical analysis
The data were analyzed using the software Statistical Package for the Social Sciences (IBM SPSS Statistics, version 21.) system. We expressed all values in the text and tables as mean ± SD. Unpaired t-test, χ2 test, and Fisher exact test were used for group differences. A p value less than 0.05 was statistically significant.
RESULTS
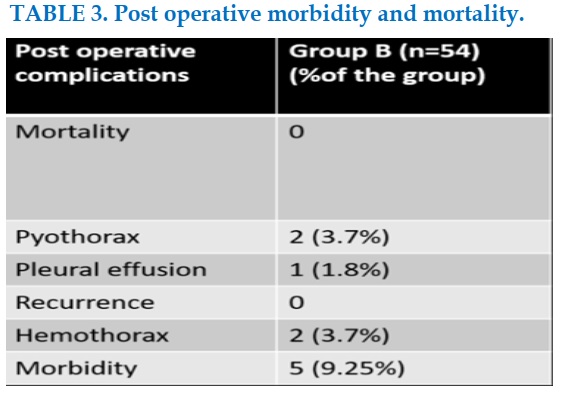
Demographic characteristics of group A and B are presented in Table 2. In the post-operative course mortality and morbidity are reported in Table 3. The functional benefit of diaphragmatic surgery is reported in the table VI.
The median duration of chest tube drainage was 2 days. In group B, 3 cases underwent a secondary operation for post operative hemothorax (n=2) and pyothorax (n=1). (Table V). No case of bronchopleural fistula occurred after the three lobectomies.
Follow-up
Few (n=7) patients were lost to follow-up, and 30 (78.9%) patients had regular follow-up. The end-point of follow-up was December 2018. The median period of follow-up was 11.5 months (range, 10-31 months; IQR, 10 months). No recurrence was noted after one year of postoperative follow-up. An improvement of the clinical respiratory and digestive symptomatology was noted in 29 cases (78%) based on a satisfactory classical questionnaire. In the group A, only 11 patients ( 22.9%) reported an objective improvement after medical therapy ( mainly functional rehabilitation). The difference between the two groups is statistically significant (p=0.025).
DISCUSSION
Diaphragmatic eventration is a rare condition, between 0.2 % [1,2]. About four men for a woman and it is described in almost 80% of cases on the left side. Clinically, diaphragmatic hernias are most often incidental discovery but large forms with diaphragmatic « hernia » cause more frequently symptomatic. For anatomic reasons (the liver mass) , right DE is more associated with respiratory symptoms such as coughing, atelectasis or recurrent pneumonia, and consequently practicians can easily consider others primary lung disease and misdiagnose the diaphragmatic disorder but left DE are more observable and known to present with post prandial digestive symptoms like pyrosis, gastrooeasophageal reflux responsible for a disorder of gastric emptying, but clinical compressive cardiac disorders are symmetrically described in both sides and are the results of the mediastinal shift [3-5]. Respiratory failure can results from multifactorial changes in respirator physiology involving atelectasis and ventilation/perfusion dysfunction toward the contralateral lung.
Apart from congenital forms of DE, those of the adult often acquired and result from muscular paralysis due to traumatic phrenic nerve injury or external nerve compression or even from a tumor or inflammatory condition of the phrenic nerve itself or by its cryofixation during of cardiac surgery [6-8]. Sometimes the DE is idiopathic when no classical etiologies were found. Some authors have suggested a degenerative origin of the nerve [9,10]. In our patients, the absence of a history of cervico-thoracic trauma, inflammatory or mediastinal tumoral pathology (excluded patients) and obvious cause on the thoracic imaging and intraoperatively led us to conclude that it is idiopathic even though we did not functionally explore the phrenic nerve.
Chest imaging (chest X-ray, CT, MRI) confirms the diagnosis by showing the diaphragmatic ascent without detectable interruption.
Digestive opacifications are less frequently used. The operative indication is always discussed if there is a functional repercussion as in our patients of group B [11,12].
The thoracic approach is guided by the clinical and radiological data and can reduce the diaphragm surface by a simple plication suture, probably, when needed, reinforced by a prosthesis depending of the muscle quality.
After the plication, the diaphragm placed in a in a lower position allow more expansion of the hemithorax and improves lung function parameters. Frequently, a decrease is observed in FVC and FEV1, which are among the restrictive-type respiratory failure parameters in the diaphragm function disorder.
Some authors performed celioscopic gastropexy [13,14]. We hard disagree with this selective surgery witch aim the digestive part of the question and unrecognized the respirator and cardiac associated symptoms. Video-assisted thoracoscopic repair offers the advantage, to easily achieve diaphragmatic plication according to the various methods currently available, double suture, U-suture or very rarely stapling by endo-GIA [6,7,15].
Most of the studies showed that surgical treatment offer different results based on subjective patient satisfaction. In our study we hope that the present comparative results even with a predominant thoracotomy use, the place of surgery is more indicated. Such what proposed Ozkan et coll [16], we also can propose a new calculation formula of what we call diaphragmatic factor DF toward :
The DF= FEV1 (L) /A, where A (Figure 1) is the distance between the two diaphragmatic cupola in deep inspiration to detection of the eventration level with digital data, may begin a new approach of multiple discussions about surgical indications. we didn’t use this formula in our study because of the retrospective appraoch and numerous missing chest radiograph in deep inspiration.
CONCLUSION
Diaphragmatic eventration is a rare condition, more frequent and more expressive on the left than on the right side. It is often related to phrenic nerve palsy in adults. In the absence of an obvious cause, we speak of idiopathic diaphragmatic herniation. Surgical treatment is required to improve functional impact.
CONFLIT OF INTEREST
The authors declare no conflict of interests.
REFERENCES
1. R.K. Freeman, T.C. Wozniak, E.B. Fitzgerald, Functional and physiologic results of video-assisted thoracoscopic diaphragm plication in adult patients with unilateral diaphragm paralysis, Ann. Thorac. Surg. 2006 ; 81:1853–1857.
2. S.M. Higgs, A. Hussain, M. Jackson, R.J. Donnelly, R.G. Berrisford, Longterm results of diaphragmatic plication for unilateral diaphragm paralysis, Eur. J. Cardiothorac. Surg. 2002 ; 21 :294–297.
3. T.P. Hu¨ttl, M.W. Wichmann, B. Reichart, T.K. Geiger, F.W. Schildberg, G. Meyer, Laparoscopic diaphragmatic plication, long-term results of a novel technique for postoperative phrenic nerve palsy, Surg. Endosc. 2004 ;18 : 547–551.
4. Z. Hwang, J.S. Shin, Y.H. Cho, K. Sun, I.S. Lee, A simple technique for the thoracoscopic plication of the diaphragm, Chest 124 (2003) 376–378.
5. M.H. Hines, Video-assisted diaphragm plication in children, Ann. Thorac. Surg. 2003 ;76 :234–236.
6. M.L. Rogers, J.P. Duffy, Surgical aspects of chronic postthoracotomy pain. A review article, Eur. J. Cardiothoracic. Surg. 2000 ; 18 :711–716.
7. Yazıcı M, Karaca ˙I, Arıkan A, et al. Congenital eventration of the diaphragm in children: 25 years’ experience in three pediatric surgery centers. Eur J Pediatr Surg 2003;13:298–301.
8. F. Gharagozloo, S.D. McReynolds, L. Snyder, Thoracoscopic plication of the diaphragm, Surg. Endosc. 1995;9 : 1204–1206.
9. Huttl TP, Wichmann MW, Reichart B, et al. Laparoscopic diaphragmatic plication: long-term results of a surgical technique for postoperative phrenic nerve palsy. Surg Endosc 2004;18:547–51.
10. Freeman RK, Wozniak TC, Fitzgerald EB. Functional and physiologic results of video-assisted thoracoscopic diaphragm plication in adult patients with unilateral diaphragm paralysis. Ann Thorac Surg. 2006;81:1853-1857.
11. Tiryaki T, Livanelio_glu Z, Atayurt H. Eventration of the diaphragm. Asian J Surg. 2006;29:8-10.
12. Versteegh MI, Braun J, Voigt PG, et al. Diaphragm plication in adult patients with diaphragm paralysis leads to long term improvement of pulmonary function and level of dyspnea. Eur J Cardiothorac Surg. 2007;32:449-456.
13. Groth SS, Andrade RS. Diaphragmatic eventration. Thorac Surg Clin 2009;19:511–9.
14. Groth SS, Rueth NM, Kast T, et al. Laparoscopic diaphragm plication for diaphragmatic paralysis and eventration: an objective evaluation of short- and mid-term results. J Thorac Cardiovasc Surg 2010;139:1452– 6.
15. Phadnis J, Pilling JE, Evans TW, Goldstraw P. Abdominal compartment syndrome: a rare complication of plication of the diaphragm. Ann Thorac Surg 2006;82:334 – 6.
16. Serdar Özkan, Ülkü Yazici,Ertan Aydin and Nurettin Karaoğlanoğlu. Is surgical plication necessary in diaphragm eventration?. Asian Journal of Surgery (2016). Vol. 39 URL
FIGURES - TABLES
REFERENCES
1. R.K. Freeman, T.C. Wozniak, E.B. Fitzgerald, Functional and physiologic results of video-assisted thoracoscopic diaphragm plication in adult patients with unilateral diaphragm paralysis, Ann. Thorac. Surg. 2006 ; 81:1853–1857.
2. S.M. Higgs, A. Hussain, M. Jackson, R.J. Donnelly, R.G. Berrisford, Longterm results of diaphragmatic plication for unilateral diaphragm paralysis, Eur. J. Cardiothorac. Surg. 2002 ; 21 :294–297.
3. T.P. Hu¨ttl, M.W. Wichmann, B. Reichart, T.K. Geiger, F.W. Schildberg, G. Meyer, Laparoscopic diaphragmatic plication, long-term results of a novel technique for postoperative phrenic nerve palsy, Surg. Endosc. 2004 ;18 : 547–551.
4. Z. Hwang, J.S. Shin, Y.H. Cho, K. Sun, I.S. Lee, A simple technique for the thoracoscopic plication of the diaphragm, Chest 124 (2003) 376–378.
5. M.H. Hines, Video-assisted diaphragm plication in children, Ann. Thorac. Surg. 2003 ;76 :234–236.
6. M.L. Rogers, J.P. Duffy, Surgical aspects of chronic postthoracotomy pain. A review article, Eur. J. Cardiothoracic. Surg. 2000 ; 18 :711–716.
7. Yazıcı M, Karaca ˙I, Arıkan A, et al. Congenital eventration of the diaphragm in children: 25 years’ experience in three pediatric surgery centers. Eur J Pediatr Surg 2003;13:298–301.
8. F. Gharagozloo, S.D. McReynolds, L. Snyder, Thoracoscopic plication of the diaphragm, Surg. Endosc. 1995;9 : 1204–1206.
9. Huttl TP, Wichmann MW, Reichart B, et al. Laparoscopic diaphragmatic plication: long-term results of a surgical technique for postoperative phrenic nerve palsy. Surg Endosc 2004;18:547–51.
10. Freeman RK, Wozniak TC, Fitzgerald EB. Functional and physiologic results of video-assisted thoracoscopic diaphragm plication in adult patients with unilateral diaphragm paralysis. Ann Thorac Surg. 2006;81:1853-1857.
11. Tiryaki T, Livanelio_glu Z, Atayurt H. Eventration of the diaphragm. Asian J Surg. 2006;29:8-10.
12. Versteegh MI, Braun J, Voigt PG, et al. Diaphragm plication in adult patients with diaphragm paralysis leads to long term improvement of pulmonary function and level of dyspnea. Eur J Cardiothorac Surg. 2007;32:449-456.
13. Groth SS, Andrade RS. Diaphragmatic eventration. Thorac Surg Clin 2009;19:511–9.
14. Groth SS, Rueth NM, Kast T, et al. Laparoscopic diaphragm plication for diaphragmatic paralysis and eventration: an objective evaluation of short- and mid-term results. J Thorac Cardiovasc Surg 2010;139:1452– 6.
15. Phadnis J, Pilling JE, Evans TW, Goldstraw P. Abdominal compartment syndrome: a rare complication of plication of the diaphragm. Ann Thorac Surg 2006;82:334 – 6.
16. Serdar Özkan, Ülkü Yazici,Ertan Aydin and Nurettin Karaoğlanoğlu. Is surgical plication necessary in diaphragm eventration?. Asian Journal of Surgery (2016). Vol. 39 URL