
 English
English
 French
French
Study of clinical and polygraphy characteristics of children with tonsillar hypertrophy and OSA
Etude des caractéristiques cliniques et polygraphiques chez les enfants atteints d’hypertrophie amygdalienne et d’AOS
Dien Tran-Minh1*, Anh Phi-Quynh1*, Phuc Nguyen-Dinh2, Sy Duong-Quy3,4
*: Co-First Authors
1: ENT Department. National Pediatric Hospital. Hanoi, Vietnam
2: ENT Department. National Hospital of ENT. Hanoi, Vietnam
3: Lam Dong Medical College. Dalat, Vietnam.
4: Department of Immuno-Allergology. Penn State Medical College. USA
Corresponding author
Dr. PHI QUYNH Anh
ENT Department. National Pediatric Hospital. Hanoi, Vietnam.
E-mail: phiquynhanhent@gmail.com
DOI: 10.12699/jfvpulm.12.37.2021.20
Introduction. Obstructive sleep apnea (OSA) can occur at any childhood period and it is very common between 2 and 8 years old due to the development of lymphoma tissue around upper respiratory tract.
Methods. It was a descriptive study. Children having all the following criteria were included in the present study: tonsillar hypertrophy, OSA, aged from 2 to12 years old.
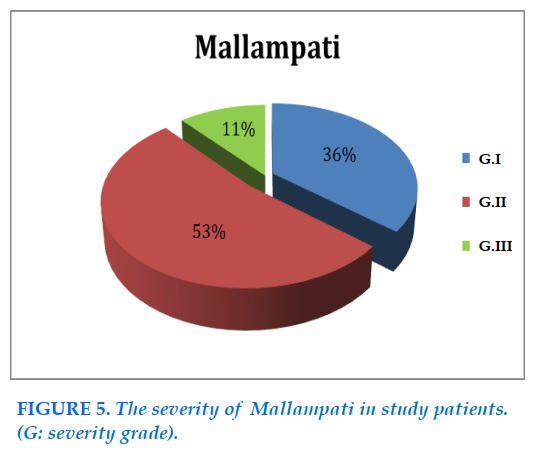
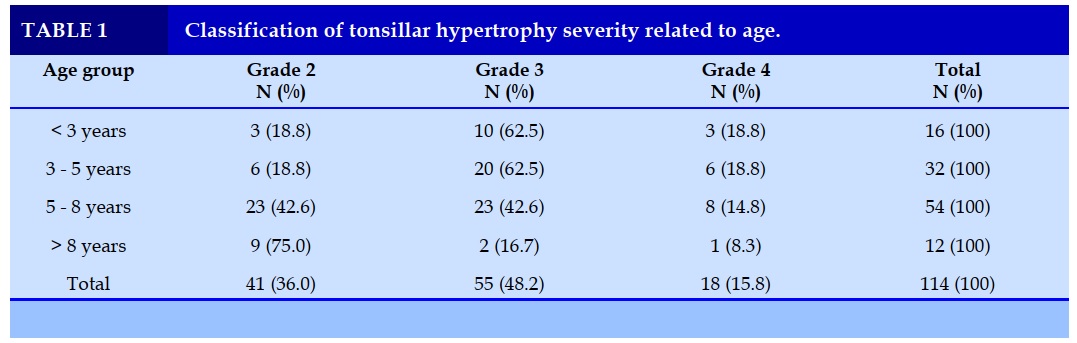
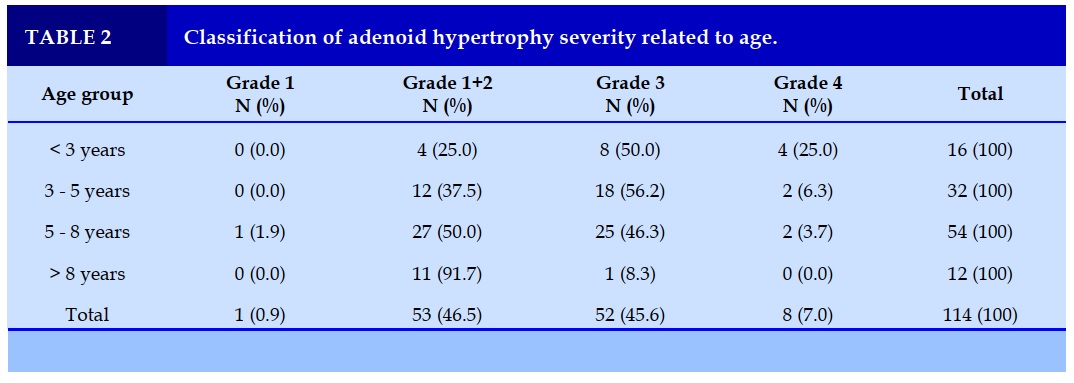
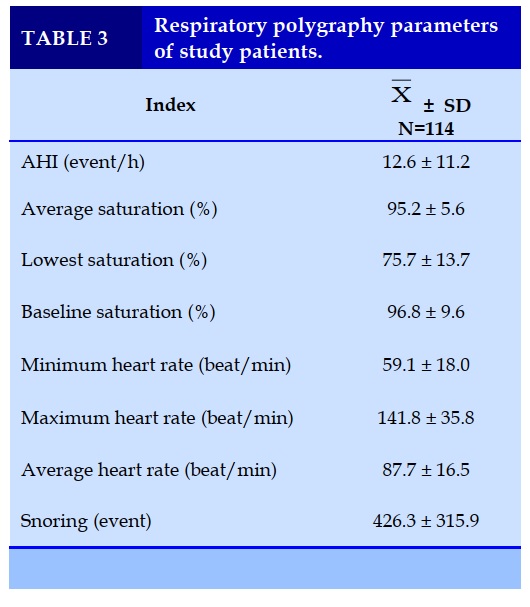
Results. There were 114 patients (2–12 years old) with mean age of 5.5±2.1 years old with the most predominant age group was 3–8 years old (75.5%); gender rate was 3.1/1 (male/female). The common symptoms were snoring (97.6%), sleep with mouth breathing (98.1%), hard breathing or heavy breathing (95.6%). The classification of tonsillar hypertrophy was: grade II: 36%, grade III: 48.2% with most common at the age from 3 to 8 years old (75.4%). The adenoid hypertrophy grade II was 46.5% vs 45.6% for grade III. There was 53% of patients having Mallampati grade II. The distribution of OSA severity was severe (38.6%), moderate (19.3%) and mild (42.1%). Average apnea hypopnea index was 12.6±11.2 event/h; lowest saturation was 75.7±13.7%; mean heart rate was 87.7±16.5 events/hour; snoring episodes was 426.3± 315.9 events.
Conclusion. Children with OSA and tonsillar hypertrophy usually have typical clinical symptom and respiratory polygraphy. Therefore, OSA should be screened and diagnosed in children who have the symptoms of OSA.
KEYWORDS: OSA; Tonsillar hypertrophy; Adenoid hypertrophy; AHI; Snoring.
Introduction. L'apnée obstructive du sommeil (AOS) peut survenir à n'importe quelle période de l'enfance et elle est très fréquente entre 2 et 8 ans en raison du développement de tissu lymphome autour des voies respiratoires supérieures.
Méthodes. Il s'agissait d'une étude descriptive. Des enfants présentant tous les critères suivants ont été inclus dans la présente étude: hypertrophie amygdalienne, AOS, âgés de 2 à 12 ans.
Résultats. Il y avait 114 patients (2 – 12 ans) avec un âge moyen de 5,5 ± 2,1 ans avec le groupe d'âge le plus prédominant était de 3 - 8 ans (75,5 %); le rapport de genre était de 3,1/1 (homme/femme). Les symptômes communs étaient le ronflement (97,6%), le sommeil avec respiration buccale (98,1%), la respiration difficile ou la respiration lourde (95,6%). La classification de l'hypertrophie amygdalienne était: grade II: 36 %, grade III: 48,2 % avec la plus fréquente à l'âge de 3 à 8 ans (75,4 %). L'hypertrophie adénoïde grade II était de 46,5% vs 45,6% pour le grade III. Il y avait 53 % de patients ayant un grade II de Mallampati. La distribution de la sévérité de l'AOS était sévère (38,6%), modérée (19,3%) et légère (42,1%). L'indice moyen d'apnée - hypopnée était de 12,6 ± 11,2 événements/h; la saturation la plus faible était de 75,7 ± 13,7 %; la fréquence cardiaque moyenne était de 87,7 ± 16,5 événements/heure; épisodes de ronflement était de 426,3 ± 315,9 événements.
Conclusion. Les enfants atteints d'AOS et d'hypertrophie amygdalienne présentent généralement des symptômes cliniques typiques et une polygraphie respiratoire. Par conséquent, l'AOS doit être dépisté et diagnostiqué chez les enfants qui présentent les symptômes de l'AOS.
MOTS CLÉS: AOS; Hypertrophie amygdalienne; Hypertrophie végétation; IAH; Ronflement.
INTRODUCTION
Obstructive sleep apnea (OSA) is a chronic obstruction of the upper airway during sleep, leading to intermittent hypoxia, oxidative stress production, and sleep fragmentation [1]. The prevalence of OSA in childhood is roughly 1-3% and depending on diagnostic criteria. However, OSA can occur at any childhood period and it is very common between 2 and 8 years old due to the development of lymphoma tissue around upper respiratory tract [2].
OSA may have a harmful impact and serious consequence on health without prompt diagnosis and treatment. Children with OSA can suffer from attension decifit hyperactivity, depression, lack of concentration, and daytime sleepiness [3]. Previous studies showed that severe OSA may induce sudden death at night in children [5,6]. In addition, recent publications also demonstrate that OSA is an independent risk factor for cardiovascular diseases such as myocardiac infraction and hypertension when children grow up [7,8].
In children, a main cause of OSA are adenotonsillar hypertrophy and vegetations adenoides, which induce the obstruction of the upper airway; therefore, a curable treatment is adenotonsillectomy. That kind of intervention is very effective in OSA children with success rate varied from 82% to 100% in different studies [9]. Therfore, this study was conducted to describe the clinical and functional characteristics of children with tonsillar or adenoid hypertrophy having OSA.
METHODS
Subjects
There were 114 children from 3 to 12 years old included in the present study in National Pediatric Hospital in Vietnam. The present study was approved by Ethical Committee of Hanoi Medical University and National Pediatric Hospital.
Inclusion criteria
Children having all the following criteria were included in the present study: tonsillar hypertrophy, OSA defined by AASM (American Academic of Sleep Medicine), aged from 2 to12 years old, and agreement from patients and their guardians.
Exclusion criteria
Children having one of the following criteria were excluded from the study: cranial-facial abnormal structure, microcrania, other disorders of the upper airway, neuro-muscular junction disorder such as myasthenia gravis, coagulopathy, renal failure, heart failure, or disagreement from patients and their guardians.
Methods
Polygraphy (PG)
OSA was defined with polygraphy by using the apnea – hypopnea index (AHI) to classify the severity of OSA as recommended: normal (non OSA): AHI ≤ 1/h; mild OSA: 1/h < AHI ≤ 5/h; moderate OSA: 5/h < AHI ≤ 10/h; severe OSA: AHI > 10/h. Polygraphy was done with ApneaLink (ResMed; San Diego, California, USA).
Tonsil hypertrophy evaluation
There are 5 levels of tonsil hypertrophy based on the ratio of tonsil to pharynx (distance between two anterior pillars), including grade 0 (located in the cavity), grade 1: occupied < 25% of the distance between the two anterior pillars, grade 2 /3/ and 4: occupied 25-50%/ 50%-75%/ and > 75% of the distance between the two anterior pillars, respectively.
Statistical analysis
Epidata and Stada 15 were used to analyze the recorded data. Continuous variables were presented as mean ± standard deviation (SD).
RESULTS
Clinical characteristics of study patients
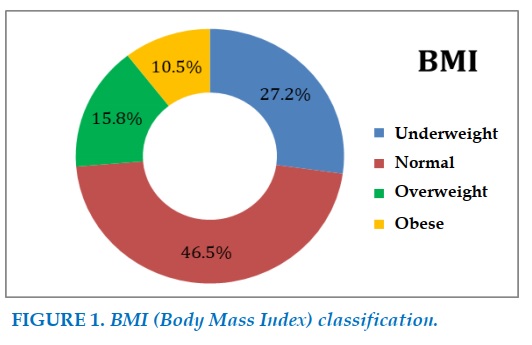
There were 114 patients (2 – 12 years old) with mean age of 5.5 ± 2.1 years old with the most predominant age group was 3 – 8 years old (75.5%); gender rate was 3.1/1 (male/female); BMI was 16.9 kg/m2. Patients underweight rate was 27.2% vs 15.8% and 10.5% with overweight and obese, respectively (Figure 1).
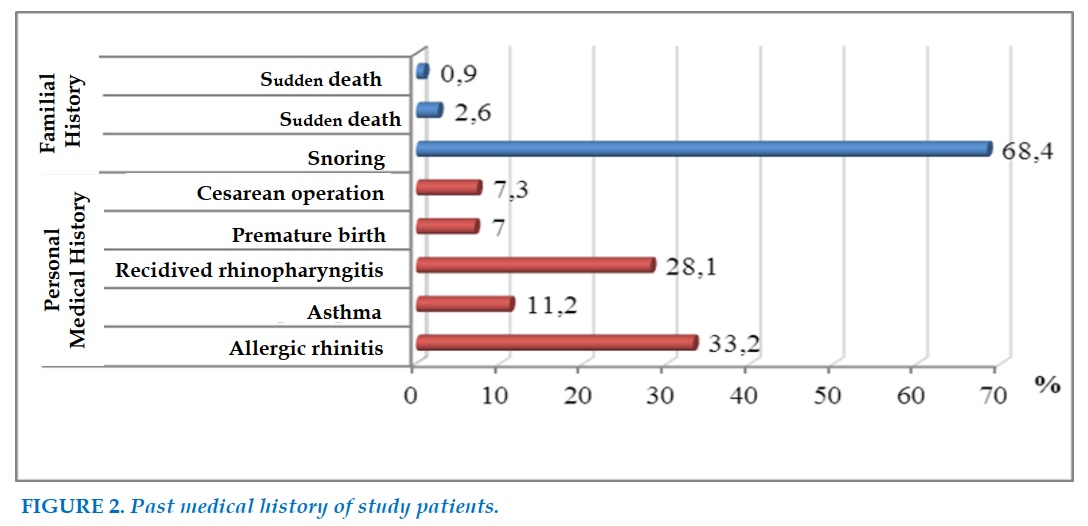
There were 33.2% of patients had in their medical history allergic rhinitis, 11.2% with asthma, 28.1% with recidived rhinopharyngitis, 7.0% with premature birth, 68.4% having snoring parents or grand-parents; among them 2.6% had OSA (Figure 2).
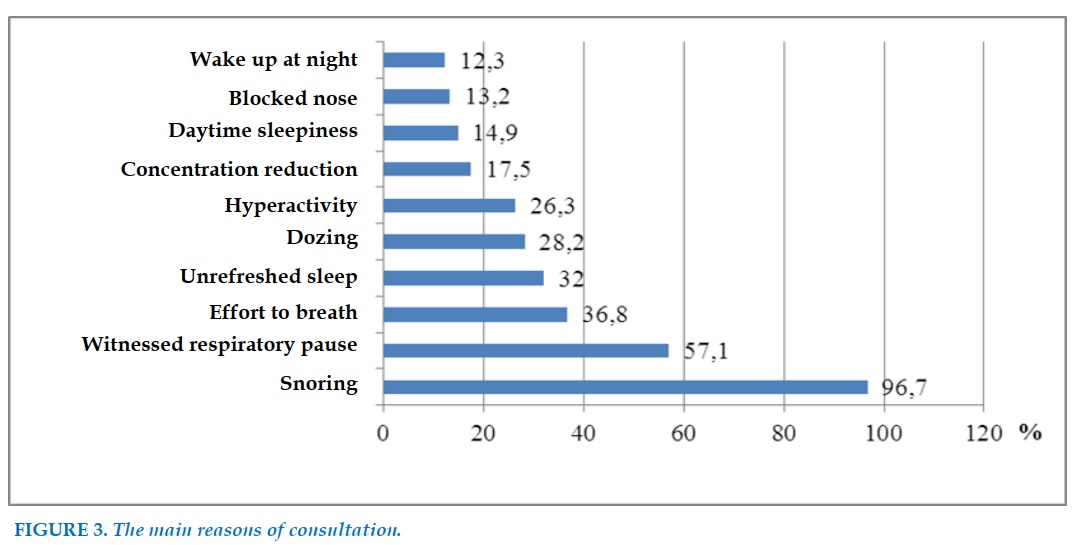
The main reasons of consultations were snoring (96.7%), pause of breathing (57.1%), effort to breath (36.8%), unrefresh sleep (32%), doze (28.2%), hyperactivity (26.3%), loss of concentration (17.5%), daytime sleepiness (14.9%), nasal congestion nose at night (13.2%), and wake up during sleep (12.3%) (Figure 3).
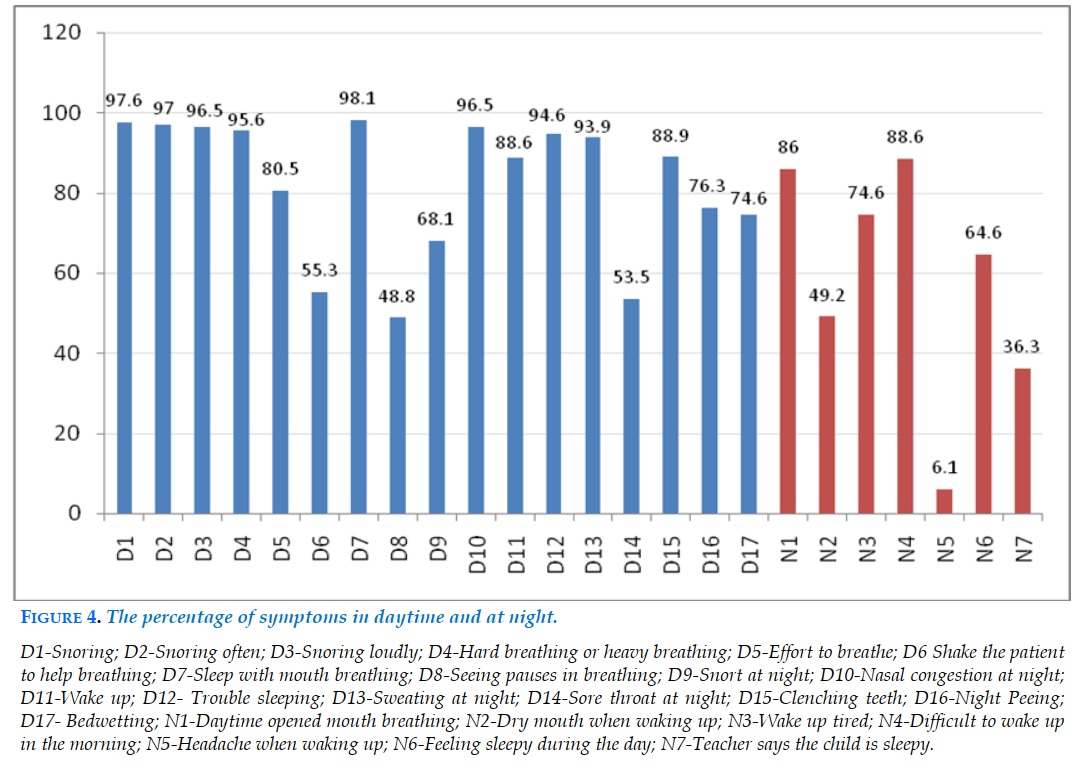
The percentage of symptoms in daytime and at night was presented in Figure 4. The common symptoms were snoring (97.6%), sleep with mouth breathing (98.1%), Hard breathing or heavy breathing (95.6%); an uncommon symptom was headache when waking up (6.1%) (Figure 4).
ENT (Ear-Nose-Throat) examination characteristics
The classification of tonsillar hypertrophy was as followed (Table 1): tonsillar hypertrophy grade II: 36%, grade III: 48.2% with most common at the age from 3 to 8 years old (75.4%).
The adenoid hypertrophy grade II was 46.5% vs 45.6% for grade III (Table 2).
The severity of Mallampati was presented in Figure 5. There was 53% of patients having Mallampati grade II (Figure 5).
Respiratory polygraphy of study patients
The distribution of OSA severity was severe (38.6%), moderate (19.3%) and mild (42.1%).
Average apnea hypopnea index was 12.6 ± 11.2 event/h; lowest saturation was75.7 ± 13.7%.
The mean heart rate was 87.7 ± 16.5 events/hour. The results showed that snoring episodes was 426.3 ± 315.9 events (Table 3).
DISCUSSION
In our study, the highest incidence of OSAS is between 2 and 8 years of age, parallel with the development of lymphatic tissue around the airways during this period. During school age and adolescence, OSA is often associated with obesity [10-11]. The number of male patients with sleep apnea is more than that of female patients, the ratio of male/female in the present study was 3/1.
Most studies in the world in both adults and children show that the prevalence of OSAS is higher in men than in women. Ronen et al., when studying the influence of gender and age on the length development of the upper airway, found that at puberty, the upper airway in boys is longer than in girls. This partly explains the higher prevalence of OSAS in post-pubertal boys and adults than in girls [12].
In children, studies of snoring and OSA showed significant differences in prevalence by sex. Snoring is considered the most basic and important symptom of OSA. In our study, snoring accounted for the highest rate up to 97.6%, there was no difference between boy and girl. This result is consistent with the observation of many other studies that the presence of snoring is significant in the diagnosis of obstructive sleep apnea syndrome. Studies by most authors show that young parents report this symptom in >85% of cases. Loud snoring, frequent snoring is the main reason why parents take their children to the doctor because it affects the quality of life of the patient as well as the family.
However, if only snoring is present, it is not possible to distinguish between children with OSA and children who snore alone. Our results showed that up to 95.6% of children with symptoms of shortness of breath or heavy breathing and 80.5% of children with apnea were witnessed at different frequencies. This apnea is often witnessed by a parent, or a sleeping relative. Eyewitnesses often share the same feeling of anxiety as to whether the child will be able to breathe again and often wake the child (Figure 3).
In our study, the rate of children having trouble sleeping and waking up was 88.6% and 94.6%. Prolonged insomnia is a symptom of OSA because sleep efficiency is reduced, patients have to wake up many times during the night. Children often turn over to adapt to hypoxia due to congestion. According to Ramsay, this symptom is related to increased breathing during apnea [13].
In our study, nocturia and bedwetting were also common symptoms with the rate of 74.6% and 86.0%, respectively (Figure 4). The mechanism of this symptom is explained by intermittent nocturnal hypoxia in patients with sympathetic nervous system-stimulating OSA, together with increased intra-abdominal pressure and increased secretion of atrial natriuretic peptide and decreased antidiuretic hormone leading to nocturia [13-17]. Our result was different from other authors, possibly because our study subjects are children. Children with central, peripheral, sympathetic, and parasympathetic nervous systems are all in the development and maturation stages, so they are easily affected by stimuli [18].
Mouth breathing due to blocked nose and dry mouth in the morning were also the common complaints of young parents in our study, accounting for quite high rates of 86% and 49.2% (Figure 4).
This symptom was related to tonsillar – adenoid hyperthophy and allergic rhinitis. Excessive daytime sleepiness is both a symptom and a consequence of obstructive sleep apnea.
Children may fall asleep or fall asleep while studying, playing or eating. Parents or relatives observed or teachers taught children reflect this phenomenon. Older children may complain of feeling drowsy. We experienced this symptom in 49.2% of children reported by teachers and 86.0% observed by parents (Figure 4).
Gozal and Melendres, investigating the association between daytime sleepiness in children and severity of OSA in two independent studies, demonstrated that daytime sleepiness was correlated with BMI, blood pressure, and OSA severity. However, in contrast to adults, daytime somnolence occurs with a lower frequency in children [19,20]. Neurological abnormalities and behavioral abnormalities are also common in children. Symptoms included decreased concentration, decreased attention, memory impairment, and mood changes (Figure 4). These factors might affect the quality of life and development of children. Hence, the screening of OSA in children and adult should be done in accredited sleep lab [21].
CONCLUSION
Children with OSA and tonsillar hypertrophy usually have typical clinical symptom such as snoring, mouth breathing, breathing effort and pauses in breathing at night, and respiratory polygraphy, including high apnea-hypopnea index and desaturation at night. Therefore, OSA should be screened and diagnosed in children who have the symptoms of OSA.
CONFLICT OF INTERESTS
Non.
REFERENCE
1. C. L. Marcus, L. J. Brooks, K. A. Draper et al.. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2012, 130 (3), 576-584.
2. Guilleminault C et al. Adenotonsillectomy and obstructive sleep apnea in children: a prospective survey. Otolaryngol Head Neck Surg 2007,136(2),169-175.
3. J. Murugesh. Obstructive Sleep Apnea in Children: Exploring the Role of Dentists in Diagnosis and Treatment. International Journal of Dental Sciences and Research 2014, 2, 12-16.
4. Riva Tauman và David Gozal. Obstructive Sleep Apnea Syndroma in children. Expert Rev Resp Med 2011, 5 (3), 425-440.
5. Redline S, Tishler P.V, Schluchter M et al. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med 1999, 159 (5 Pt 1), 1527-1532.
6. Arens R và Muzumdar H. Childhood obesity and obstructive sleep apnea syndrome. J Appl Physiol 2010, 108 (2), 436-444.
7. Chang S.J và Chae K.Y. Obstructive sleep apnea syndrome in children: Epidemiology, pathophysiology, diagnosis and sequelae. Korean J Pediatr 2010, 53 (10), 863-871.
8. Lam Y.Y, Chan E.Y, Chan C.H et al. The correlation among obesity, apnea-hypopnea index, and tonsil size in children. Chest 2006, 130 (6), 1751-1756.
9. Verhulst S.L, Schrauwen N, Haentjens D et al. Sleep-disordered breathing in overweight and obese children and adolescents: prevalence, characteristics and the role of fat distribution. Arch Dis Child 2007, 92 (3), 205-208.
10. Muzumdar H, Arens R. Diagnostic issues in pediatric obstructive sleep apnea. Proc Am Thorac Soc 2008, 5 (2), 263-273.
11. Arens R, Marcus C.L. Pathophysiology of upper airway obstruction: a developmental perspective. Sleep 2004, 27 (5), 997-1019.
12. Ronen O, Malhotra A, Pillar G et al. Influence of gender and age on upper-airway length during development. Pediatrics 2007, 120 (4), e1028-1034.
13. Ramsey R, Culebras A, Ivanenko A et al. History and Physical Examination, Diagnosis and Treatment Obstructive sleep Apnea. Informa Health careUSA2009;1-20.
14. Duong-Quy S, K Dang Thi Mai, N Tran Van et al. Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam. Rev Mal Respir 2018; 35(1):14-24.
15. KDT Mai, TD Vu, NT Van, ANT Hong, Duong–Quy S. Obstructive Sleep Apnea (OSA) and Metabolic Syndrome (MetS). J Func Vent Pulm 11 (33), 36-41.
16. K Bui-Diem, D Do Van, Duong-Quy S. Methods for assessing alertness and level of vigilance in patients with obstructive sleep apnea. J Func Vent Pulm 2020;11 (35), 1-6.
17. K Dang-Thi-Mai, TD Vu, NT Van, V Le Thuong, H Vu, Duong-Quy S. Study on the correlation between excessive daytime sleepiness and obstructive sleep apnea. J Func Vent Pulm 2020;34(11):28-32.
18. Christian G, Ali B. Clinical Feature ang Evaluation of Obstructive Sleep Apnea- Hyponea syndrome and upper airway resistance syndrome., Elsevier Saunders 2005.
19. Gozal D, Wang M, Pope D.W. Objective sleepiness measures in pediatric obstructive sleep apnea. Pediatrics 2001, 108 (3), 693-697.
20. Melendres M.C et al. Daytime sleepiness and hyperactivity in children with suspected sleep-disordered breathing. Pediatrics 2004, 114 (3), 768-775.
21. AS BaHammam, F Han, R Gupta, S Duong-Quy, MA Al-Abri, HA Jahrami, et al. Asian accreditation of sleep medicine physicians and technologists: practice guidelines by the Asian Society of Sleep Medicine. Sleep Medicine 2021;81, 246-252.
FIGURES - TABLES
REFERENCE
1. C. L. Marcus, L. J. Brooks, K. A. Draper et al.. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2012, 130 (3), 576-584.
2. Guilleminault C et al. Adenotonsillectomy and obstructive sleep apnea in children: a prospective survey. Otolaryngol Head Neck Surg 2007,136(2),169-175.
3. J. Murugesh. Obstructive Sleep Apnea in Children: Exploring the Role of Dentists in Diagnosis and Treatment. International Journal of Dental Sciences and Research 2014, 2, 12-16.
4. Riva Tauman và David Gozal. Obstructive Sleep Apnea Syndroma in children. Expert Rev Resp Med 2011, 5 (3), 425-440.
5. Redline S, Tishler P.V, Schluchter M et al. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med 1999, 159 (5 Pt 1), 1527-1532.
6. Arens R và Muzumdar H. Childhood obesity and obstructive sleep apnea syndrome. J Appl Physiol 2010, 108 (2), 436-444.
7. Chang S.J và Chae K.Y. Obstructive sleep apnea syndrome in children: Epidemiology, pathophysiology, diagnosis and sequelae. Korean J Pediatr 2010, 53 (10), 863-871.
8. Lam Y.Y, Chan E.Y, Chan C.H et al. The correlation among obesity, apnea-hypopnea index, and tonsil size in children. Chest 2006, 130 (6), 1751-1756.
9. Verhulst S.L, Schrauwen N, Haentjens D et al. Sleep-disordered breathing in overweight and obese children and adolescents: prevalence, characteristics and the role of fat distribution. Arch Dis Child 2007, 92 (3), 205-208.
10. Muzumdar H, Arens R. Diagnostic issues in pediatric obstructive sleep apnea. Proc Am Thorac Soc 2008, 5 (2), 263-273.
11. Arens R, Marcus C.L. Pathophysiology of upper airway obstruction: a developmental perspective. Sleep 2004, 27 (5), 997-1019.
12. Ronen O, Malhotra A, Pillar G et al. Influence of gender and age on upper-airway length during development. Pediatrics 2007, 120 (4), e1028-1034.
13. Ramsey R, Culebras A, Ivanenko A et al. History and Physical Examination, Diagnosis and Treatment Obstructive sleep Apnea. Informa Health careUSA2009;1-20.
14. Duong-Quy S, K Dang Thi Mai, N Tran Van et al. Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam. Rev Mal Respir 2018; 35(1):14-24.
15. KDT Mai, TD Vu, NT Van, ANT Hong, Duong–Quy S. Obstructive Sleep Apnea (OSA) and Metabolic Syndrome (MetS). J Func Vent Pulm 11 (33), 36-41.
16. K Bui-Diem, D Do Van, Duong-Quy S. Methods for assessing alertness and level of vigilance in patients with obstructive sleep apnea. J Func Vent Pulm 2020;11 (35), 1-6.
17. K Dang-Thi-Mai, TD Vu, NT Van, V Le Thuong, H Vu, Duong-Quy S. Study on the correlation between excessive daytime sleepiness and obstructive sleep apnea. J Func Vent Pulm 2020;34(11):28-32.
18. Christian G, Ali B. Clinical Feature ang Evaluation of Obstructive Sleep Apnea- Hyponea syndrome and upper airway resistance syndrome., Elsevier Saunders 2005.
19. Gozal D, Wang M, Pope D.W. Objective sleepiness measures in pediatric obstructive sleep apnea. Pediatrics 2001, 108 (3), 693-697.
20. Melendres M.C et al. Daytime sleepiness and hyperactivity in children with suspected sleep-disordered breathing. Pediatrics 2004, 114 (3), 768-775.
21. AS BaHammam, F Han, R Gupta, S Duong-Quy, MA Al-Abri, HA Jahrami, et al. Asian accreditation of sleep medicine physicians and technologists: practice guidelines by the Asian Society of Sleep Medicine. Sleep Medicine 2021;81, 246-252.
ARTICLE INFO
DOI: 10.12699/jfvpulm.12.37.2021.20
Conflict of Interest
Non
Date of manuscript receiving
15/3/2021
Date of publication after correction
15/7/2021
Article citation
Tran-Minh D, Phi-Quynh A, Nguyen-Dinh P. Duong-Quy S. Study of clinical and polygraphy characteristics of children with tonsillar hypertrophy and OSA. J Func Vent Pulm 2021;37(12):20-25