
 English
English
 French
French
Study clinical, paraclinical features and the outcome of treatment for neonatal infections in early period at Ninh Thuan provincial general hospital
Étudier les caractéristiques cliniques, paracliniques et les résultats du traitement des infections néonatales en période précoce à l'hôpital général provincial de Ninh Thuan
Le Huy Thach1, Phan Hung Viet2, Le Van Thanh1, Phan Nguyen Quang Tung1
1: Ninh Thuan provincial general hospital
2: Hue University of Medicine and Pharmacy
Corresponding author
Dr. Le Huy Thach
L’Hôpital Général Provincial Ninh Thuan. Ninh Thuan province. Vietnam
E-mail: lh.thach67@gmail.com
DOI: 10.12699/jfvpulm.12.37.2021.26
ABSTRACT
Introduction. Neonatal infection early period is a major cause of mortality and morbidity.
Objective. Describe clinical, paraclinical features and the outcome of treatment early period neonatal infection. Design of Longitudinal study. Including 131 infants from 1 to 7 days old, treated for neonatal infections at pediatrics department, general hospital Ninh Thuan province, from February 1, 2019 to March 1, 2020.
Results. Clinical: Systemic: Pale yellow skin (13.7%), hemorrhage (13%), cyanosis (12.2%), fever (11.5%). The cardiac: heart rate ≥ 160 beats/ minute (19.8%) and < 100 beats/ minute (6.9%), CRT > 3 seconds (12,2%). Respiratory: breathing rate ≥ 60 beats/ minute (51.9%) and < 20 beats/ minute (15.3%), breathlessness (48.9%), apnea (26.0%). Neurological: decreased reflexes (47.3%), poor muscle tone (38.9%), inflexibility (24.4%), lethargy/ coma (19.8%). Gastrointestinal: poor feeding/give up breading (52.7%), vomiting (13.7%), abdominal distention (11.5%). Paraclinical: WBC < 6.000/mm3 (4.6%), > 30.000/ mm3 (7.6%). PLT < 100.000/mm3 (1.5%), > 500.000/mm3 (0.8%). CRP > 10mg/l (14.5%). Positive blood cultures was 15.3%. The mortality rate was 17.6%. Factors associated with death were poor breading/ give up breading and heart rate ≥ 160 beats/min (p<0.05).
Conclusion. The degree of clinical and Paraclinical manifestations is highly variable depending on the virulence of pathogens and on the mechanisms of host defense.
KEYWORDS: Ninh Thuan provincial general hospital; Neonatal infection
RÉSUMÉ
Introduction. L'infection néonatale en période précoce est une cause majeure de mortalité et de morbidité.
Objectif. Décrire les caractéristiques cliniques, paracliniques et les résultats du traitement de l'infection néonatale en pé-riode précoce. Conception de l'étude longitudinale. Dont 131 nourrissons de 1 à 7 jours, traités pour infections néonatales au service de pédiatrie, hôpital général de la province de Ninh Thuan, du 1er février 2019 au 1er mars 2020.
Résultats. Clinique : Systémique : Peau jaune pâle (13,7%), hémorragie (13%), cyanose (12,2%), fièvre (11,5%). Le cardiaque : fréquence cardiaque ≥ 160 battements/ minute (19,8 %) et < 100 battements/ minute (6,9 %), CRT > 3 secondes (12,2 %). Respiratoire : fréquence respiratoire ≥ 60 battements/minute (51,9 %) et < 20 battements/minute (15,3 %), essoufflement (48,9 %), apnée (26,0 %). Neurologique : diminution des réflexes (47,3%), faible tonus musculaire (38,9%), inflexibilité (24,4%), léthargie/coma (19,8%). Gastro-intestinal : mauvaise alimentation/ arrêt de la succion (52,7 %), vomissements (13,7 %), distension abdominale (11,5 %). Paraclinique : GB < 6 000/mm3 (4,6 %), > 30 000/ mm3 (7,6 %). PLT < 100 000/ mm3 (1,5 %), > 500 000/mm3 (0,8 %). CRP > 10mg/l (14,5%). Les hémocultures positives étaient de 15,3 %. Le taux de mortalité était de 17,6 %. Les facteurs associés au décès étaient une mauvaise succion/l'arrêt de la succion et une fréquence cardiaque ≥ 160 battements/min (p<0,05).
Conclusion. Le degré de manifestations cliniques et paracliniques est très variable en fonction de la virulence des pathogènes et des mécanismes de défense de l'hôte
MOTS CLÉS: Hôpital général provincial de Ninh Thuan; Infection néonatale
INTRODUCTION
Mortality in children and especially in the neonatal period is not only a concern of the health sector but
also a common concern of the whole society. According to statistics of the World Health Organization, in 2019 globally, 2.4 million children died in the first month of life. Approximately 7,000 infants die every day, accounting for 47% of all deaths of children under 5 years of age [1]. In Vietnam, there are about 18,000 newborn deaths each year, the neonatal mortality rate is 14/1000 live births, accounting for nearly 60% of the under-5 mortality rate [2]. Early neonatal sepsis is an important cause of infant mortality and morbidity.
Given the high mortality rate, identifying and caring for infants with infections can be one of the biggest
challenges facing healthcare providers. In hospitals, bacterial infections always occupy an important place in the morbidity pattern as well as the cause of death in the early neonatal period. A study at Tien Giang General Hospital (2015), showed that neonatal infection accounted for 24.25% in the neonatal morbidity model and the neonatal mortality rate was 7.35% [3].
Neonatal sepsis is considered an emergency diagnosis. However, the clinical features are very diverse, easy to confuse with other diseases, bacteriological tests often have late results. Therefore, the combination of taking maternal history, clinical signs as well as the support of blood and biochemical tests, has played an important role in the early diagnosis of infection. Ninh Thuan Provincial General Hospital with a scale of 1000 beds for patients, where newborns are examined and cared for by doctors right from the moment they are born. Therefore, consolidating and simultaneously improving the quality of neonatal care, contributing to improving treatment, staff training, and coordination between the obstetrics and pediatrics departments through research is very necessary.
Stemming from that fact, we conducted this study to describe the clinical, subclinical characteristics, treatment results, and factors affecting the results of treatment of neonatal sepsis in the first stage. premature birth at Ninh Thuan Provincial General Hospital.
METHODS
Study subject
131 infants aged 1-7 days old, treated for neonatal infections at the Pediatric Department of Ninh Thuan General Hospital from February 1, 2019, to March 1, 2020. Criteria for selection of patients Infants in the early neonatal period from 1-7 days of age, consistent with the diagnostic criteria for possible infectious disease (ANAES) according to ANAES [4], adjusted by CHU Toulouse [5]. Diagnostic criteria are based on 3 factors: risk factors, clinical, and laboratory.
Exclusion Criteria
No clinical symptoms or clinical symptoms but improvement without use or change of antibiotics.
There were no changes in laboratory tests of early neonatal sepsis.
Methods
Study Design
A longitudinal follow-up study.
Sample size and sampling method. Convenient sample size and follow-up method.
Steps to conduct research
Select the disease according to the criteria of history, clinical examination. Conduct complete blood count test, CRP and blood cultures at hospital admission.
- Complete blood count. Take 1ml of venous blood and put it in a tube with EDTA anticoagulant. Results read on a 26-parameter hematology machine Horiba ABX Pentra XL 80.
- CRP. Take 1.5ml of venous blood and put it into a tube without EDTA anticoagulant (white cap tube).
Results read on the HumaStar 600 Human automatic biochemistry machine.
- Blood culture. Take blood before using antibiotics. If you are taking antibiotics, you must stop antibiotics or draw blood before the time of using the next antibiotic dose. Take 3-5 ml of venous blood, ensure the correct aseptic technique, do not contaminate, put in the blood culture bottle Bact/Alert FA plus. Incubate blood culture bottles in BacT Alert blood culture machine.
Record clinical, paraclinical and treatment results in a pre-designed study sheet.
Evaluation of treatment results
- Cured. Children recover from the disease with the initial course of antibiotic treatment.
Cure with adding or changing antibiotics.
- Death (Death at the hospital and/or severe return home).
Processing and analyzing data
Data was entered and processed using SPSS version 22.0 software. Qualitative variables are expressed as percentages (%). Use medians and percentile ranges (25 and 75) to describe quantitative variables that are not normally distributed.
Compare proportions using the When squared test or the Fisher test in the case of violating the assumption of the When squared test. Calculate the odds ratio OR and the 95% confidence interval of the OR. Compare the two mean values using the MannWhitney test in case the quantitative data are not normally distributed. Using a multivariable logistic regression model with OR value and 95% confidence interval of OR to find factors related to treatment outcome.
RESULT
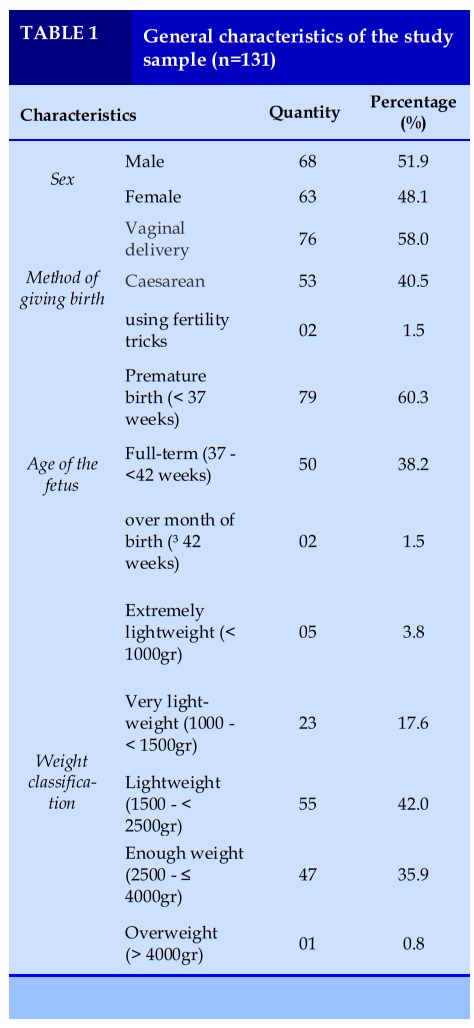
General characteristics of the study group
Children were male and female, with a male : female ratio of 1.1:1, most were born by Vaginal delivery
(58.0%), most were born prematurely (60.3%), and were born with low birth weight most common (42.0%).
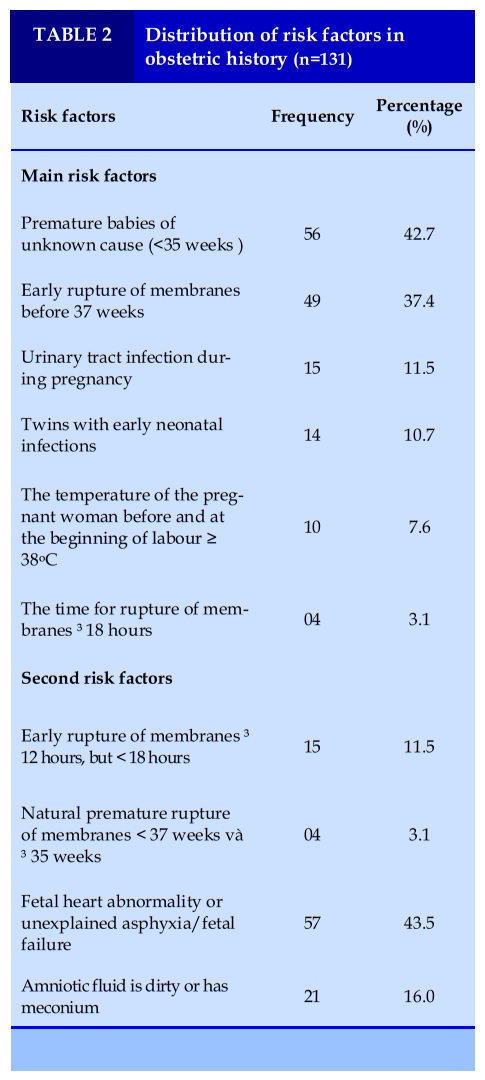
Distribution of risk factors in obstetric history
The primary risk factor with the highest incidence was unexplained preterm birth <35 weeks and the second risk factor was an abnormal fetal heart rate or unexplained asphyxia/fetal failure.
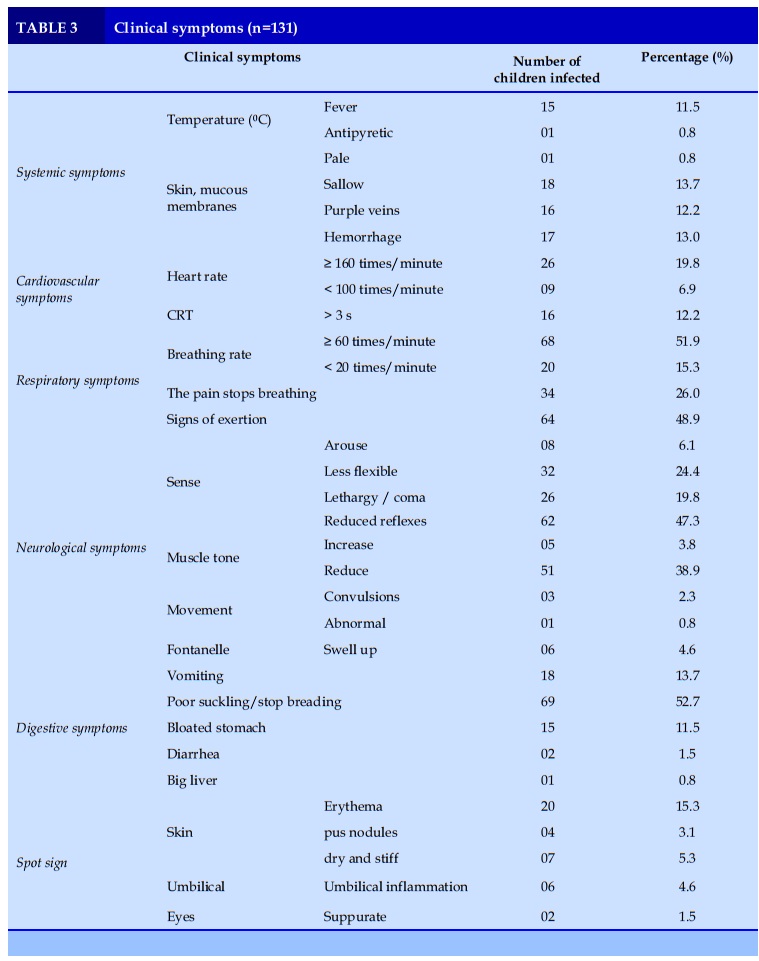
Clinical features
The most common systemic symptoms were pale yellow skin (13.7%) and hemorrhage (13%). Cardiovascular is heart rate ≥160 times/minute (19.8%) and CRT >3 seconds (12.2%). Respiration is respiratory rate ≥60 times/minute (51.9%) and exertion sign (48.9%).
Nervousness is mainly reduced reflexes (47.3%) and decreased muscle tone (38.9%). Digestion is mostly poor breading/ abstaining from suckling (52.7%). Erythema skin is the local sign with the highest rate (15.3%).
Features of paraclinical tests
The number of white blood cells decreased <6,000/mm3 accounted for 4.6% and increased >30,000/mm3 was 7.6%.
A decrease in platelet count <100,000/mm3 is 1.5% and an increase >500,000/mm3 is 0.8%. CRP >10
mg/l accounts for 14.5%. Positive blood cultures were 15.3%.
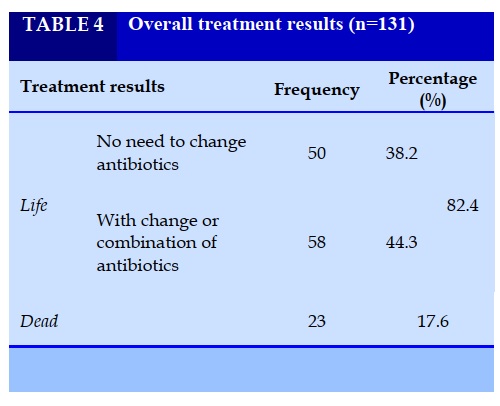
Treatment results
The mortality rate due to early neonatal infection accounted for 17.6%.
Some factors related to treatment outcome
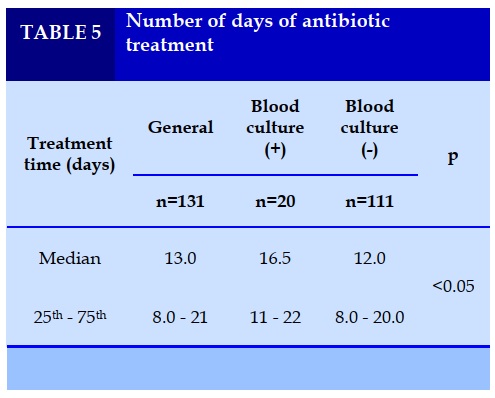
The median treatment day was 13 days, there was a significant difference in the median number of days of treatment between the two groups of positive blood cultures and negative blood cultures (p<0.05)
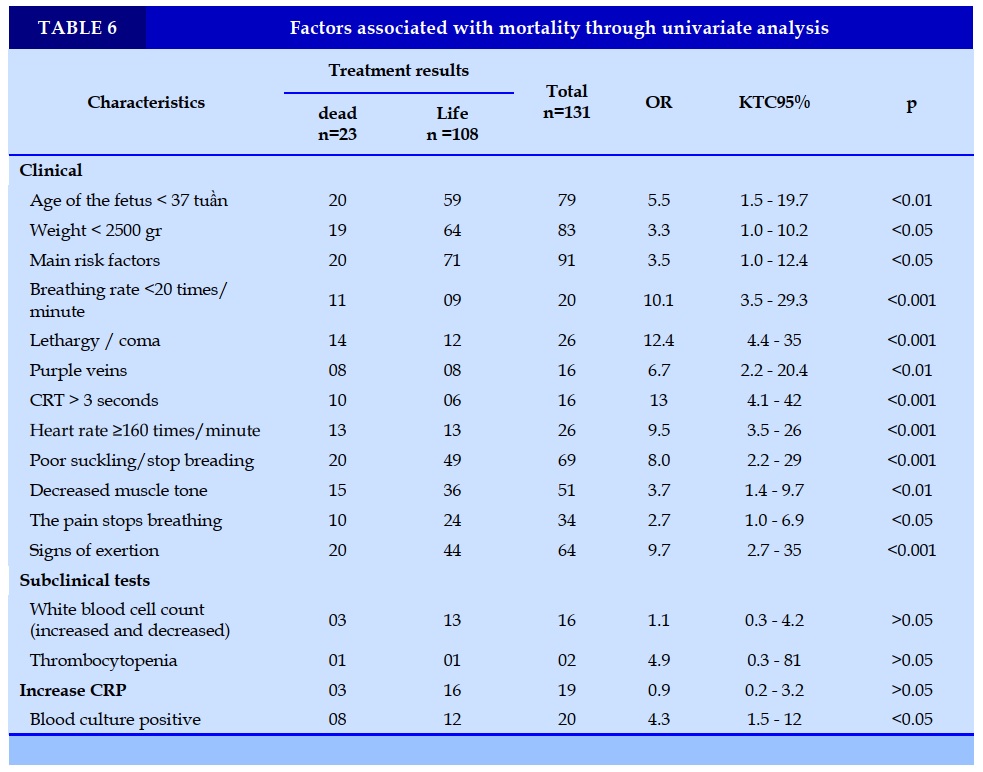
Significant clinical factors associated with mortality were fetal age <37 weeks, weight <2500 g, major risk factor, respiratory rate <20 breaths/min, lethargy/coma, cyanosis, CRT >3 s, heart rate ≥160 beats/min, poor breading/abortion, decreased muscle tone, apnea and execise signs (p<0.05). Positive blood culture was the only laboratory test associated with mortality (p<0.05).
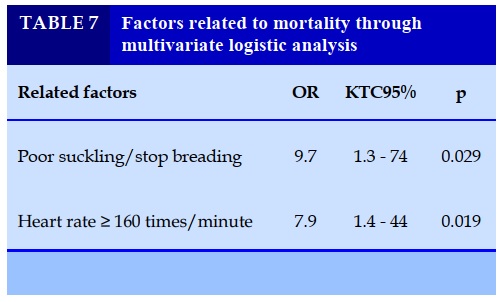
Factors that were independently associated with mortality through multivariable logistic regression analysis were poor breading/retraction (OR=9.7, p=0.029) and heart rate ≥ 160 beats/min (OR=7.9, p=0.019).
DISCUSSION
Clinical and paraclinical features
The general characteristics of the study subjects were similar to those of Tran Thi Bich Huyen, 54% boys, and 46% girls, 58% vaginal birth [6]. However, the preterm birth rate (8%) is much lower than ours. Regarding the risk factors in the obstetric history, the results showed that the main risk factors including unexplained preterm birth <35 weeks and premature rupture of membranes before 37 weeks were the two most common risk factors.
Do Ho Tinh Tam noted that the time of rupture of membranes is >18 hours (27.5%) and the mother's fever 38oC (22.1%) is the two main common risk factors, the lowest is chorioamnionitis (1.5 %) and urinary tract infections during pregnancy (3.8%) [7]. In our study, urinary tract infection during pregnancy (11.5%) and maternal fever (7.6%) were similar to Tran Quoc Viet [8]. Comparing the secondary risk factors, Do Ho Tinh Tam recorded abnormal fetal heart rate or unexplained fetal asphyxia/failure in only 8.4%, lower than us, premature rupture of membranes ≥12 hours, but <18 hours (13.7%) and dirty amniotic fluid or meconium (13.7%), similar to ours [7].
Studying 131 cases, we found that the clinical signs were different, most of them showed from 1 to many clinical signs, some cases had all the signs. According to the results in Table 3, the most common clinical signs were gastrointestinal symptoms, namely poor feeding/ abstinence (52.7%). Compared with other authors in the world and in Vietnam about signs of poor breading/stopping, we find that the rate is always high, Mhada (62.4%) [9], Vo Huu Duc, and Ta Van Tram (87.50%) [10].
In addition, the clinical features of early neonatal infection are diverse, the prevalence of signs varies
depending on the characteristics of the subjects as well as the study area. According to Tran Thi Bich
Huyen, common clinical signs are jaundice before 24 hours (32%), poor feeding, regurgitation (18%) and up to 48% of cases have no symptoms [6].
Rapid breathing is the earliest symptom of respiratory symptoms when a child has pneumonia. Do Ho
Tinh Tam, rapid breathing accounted for 42%, especially this study also showed that the rate of fever was 12.2% and hypothermia was 3.1% [7], similar to ours. Besides, our study recorded some neurological symptoms such as convulsions (2.3%), fontanelles (4.6%), similar to Mhada, convulsions (3.0%). and a bulging fontanelle (10%) [9].
Research results in only 4.6% cases with white blood cell count decreased and increased 7.6%. Tran Thi Bich Huyen also had only 2% of cases with a decrease in white blood cell count and an increase of
10% [6]. In addition, platelet counts are also suggestive of early neonatal infection, but not always with a high rate of variation.
Similar to us, Do Ho Tinh Tam recorded a 13% decrease in platelets and no cases of thrombocytosis [7]. CRP value reflects infection in the early stage, in our study, CRP >10 mg/l accounted for 14.5%, similar to Tran Thi Bich Huyen, CRP >10-20 has a rate of 18 % [6]. Blood culture is the gold standard for diagnosing neonatal sepsis, with similar positive blood cultures for Kalathia (17.8%) [11].
Treatment results
The study results showed that the median treatment day was 13 days, the number of days in the positive blood culture group (16.5 days) was higher than the negative blood culture group (p<0.05). Vo Huu Duc and Ta Van Tram, treatment time for early neonatal infections from 4-14 days had the highest rate (58.3%) [10], Trinh Thu Dung averaged 12.45 days [12], Jajoo average is 17.4 days [13]. The mortality rate in our study is similar to Vo Huu Duc (15.58%) [3].
Through univariate analysis, there are many factors significantly related to mortality, however, after multivariable logistic regression analysis, there are only two factors that are independently associated with mortality, namely poor feeding/abortion. and heart rate ≥160 times/minute (p < 0.05). In Tareen's study, poor feeding was one of the risk factors for mortality (OR=7,807, p<0.001) [14]. Do Ho Tinh Tam
results in premature birth, pale yellow skin, purple lips, rapid breathing, and poor flexibility are factors
that are independently associated with poor treatment response through multivariate analysis (p<0.05) [7].
With the above results, it can be seen that in addition to the diversity of clinical manifestations, the risk
factors for mortality in the setting of early neonatal sepsis are also different. Therefore, it is necessary to closely monitor children with these manifestations in order to make timely adjustments during care and treatment, to limit neonatal mortality.
CONCLUSION
Clinical and laboratory symptoms in early neonatal sepsis are diverse, easy to confuse and miss, leading to delays in treatment. The most common symptoms are gastrointestinal, respiratory, neurological. Mortality due to early neonatal infection accounted for 17.6%. Factors associated with mortality were poor breading/retraction (OR=9.7, p=0.029) and tachycardia ≥ 160 times/minute (OR=7.9, p=0.019).
CONFLICT OF INTERESTS
Non.
REFERENCE
1. WHO (2020), Newborns: improving survival and well-being, accessed 2 December 2020 https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality.
2. World Health Organization (2015), Neonatal Health, http://www.wpro.who.int/vietnam/topics/newborn_health/factsheet/vi/.
3. Võ Hữu Đức (2015), Models of morbidity, mortality and causes of hospitalization of newborns at Tien Giang Central General Hospital in 2013-2014”, HCMC Medicine, 19(3): 36-42.
4. Agence Nationale d’Accréditation et d’Evaluation en Santé (ANAES) (2002), Diagnostic et traitement curatif de l’infection bactérienne précoce du nouveau-né, Recommandations pour la pratique clinique: 4-6.
5. Blasco V. (2017), Etude descriptive des infections bacteriennes neonatales precoce dans une maternite niveaux III avec evalution des pratiques de soins, Universite Toulouse III - Faculte de Medecine.
6. Tran Thi Bich Huyen (2013), "The situation of early neonatal infections at the University Hospital of Medicine and Pharmacy 2", City Medicine. HCM, 17(4): 93-97.
7. Do Ho Tinh Tam (2016), Research on clinical characteristics, laboratory tests and results of treatment of early neonatal infections in Pediatrics Department, Hue University of Medicine and Pharmacy, Master of Medicine Thesis, University of Medicine and Pharmacy Hue.
8. Tran Quoc Viet (2012),Research on some clinical characteristics and diagnostic value of peripheral blood leukocytes in early neonatal infections through maternal and fetal transmission at the Pediatric Department of Hue University of Medicine and Pharmacy Hospital,Thesis Specialist level II,Hue UMP.
9. Mhada TV, Fredrick F, Matee MI, et al(2012), Neonatal sepsis at Muhimbili National Hospital, Dar es Salaam, Tanzania; aetiology,antimicrobial sensitivity pattern and clinical outcome,BMC public health,12(1):904.
10. Vo Huu Duc and Ta Van Tram (2018), "Characteristics of early neonatal infections in Neonatal Intensive Care Unit, Tien Giang Central General Hospital from January 2015 to December 2016", HCM, City Medicine . 22(4): 234-238.
11. Kalathia MB, Shingala PA, Parmar PN, et al (2013), “Study of umbilical cord blood culture in diagnosis of early-onset sepsis among newborns with high-risk factors”, Journal of clinical neonatology, 2(4): 169-172.
12. Trinh Thu Dung, Huynh Thi Duy Huong and Pham Thu Thuy (2008), "10 characteristics of neonatal systemic infection syndrome in neonatology department of Bac Lieu hospital from 09/2006-04/2007", MUHCM, 12(1): 45-50.
13. Jajoo M, Kapoor K, Garg LK, et al (2015), “To study the incidence and risk factors of early onset neonatal sepsis in an out born neonatal intensive care unit of India”, Journal of Clinical Neonatology, 4(2): 91.
14. Tareen Z, Jirapradittha J, Sirivichayakul C, et al (2017), “Factors associated with mortality outcomes in neonatal septicemia in Srinagarind hospital, Thailand”, Neonat Pediatr Med, 3(131).
TABLES
REFERENCE
1. WHO (2020), Newborns: improving survival and well-being, accessed 2 December 2020 https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality.
2. World Health Organization (2015), Neonatal Health, http://www.wpro.who.int/vietnam/topics/newborn_health/factsheet/vi/.
3. Võ Hữu Đức (2015), Models of morbidity, mortality and causes of hospitalization of newborns at Tien Giang Central General Hospital in 2013-2014”, HCMC Medicine, 19(3): 36-42.
4. Agence Nationale d’Accréditation et d’Evaluation en Santé (ANAES) (2002), Diagnostic et traitement curatif de l’infection bactérienne précoce du nouveau-né, Recommandations pour la pratique clinique: 4-6.
5. Blasco V. (2017), Etude descriptive des infections bacteriennes neonatales precoce dans une maternite niveaux III avec evalution des pratiques de soins, Universite Toulouse III - Faculte de Medecine.
6. Tran Thi Bich Huyen (2013), "The situation of early neonatal infections at the University Hospital of Medicine and Pharmacy 2", City Medicine. HCM, 17(4): 93-97.
7. Do Ho Tinh Tam (2016), Research on clinical characteristics, laboratory tests and results of treatment of early neonatal infections in Pediatrics Department, Hue University of Medicine and Pharmacy, Master of Medicine Thesis, University of Medicine and Pharmacy Hue.
8. Tran Quoc Viet (2012),Research on some clinical characteristics and diagnostic value of peripheral blood leukocytes in early neonatal infections through maternal and fetal transmission at the Pediatric Department of Hue University of Medicine and Pharmacy Hospital,Thesis Specialist level II,Hue UMP.
9. Mhada TV, Fredrick F, Matee MI, et al(2012), Neonatal sepsis at Muhimbili National Hospital, Dar es Salaam, Tanzania; aetiology,antimicrobial sensitivity pattern and clinical outcome,BMC public health,12(1):904.
10. Vo Huu Duc and Ta Van Tram (2018), "Characteristics of early neonatal infections in Neonatal Intensive Care Unit, Tien Giang Central General Hospital from January 2015 to December 2016", HCM, City Medicine . 22(4): 234-238.
11. Kalathia MB, Shingala PA, Parmar PN, et al (2013), “Study of umbilical cord blood culture in diagnosis of early-onset sepsis among newborns with high-risk factors”, Journal of clinical neonatology, 2(4): 169-172.
12. Trinh Thu Dung, Huynh Thi Duy Huong and Pham Thu Thuy (2008), "10 characteristics of neonatal systemic infection syndrome in neonatology department of Bac Lieu hospital from 09/2006-04/2007", MUHCM, 12(1): 45-50.
13. Jajoo M, Kapoor K, Garg LK, et al (2015), “To study the incidence and risk factors of early onset neonatal sepsis in an out born neonatal intensive care unit of India”, Journal of Clinical Neonatology, 4(2): 91.
14. Tareen Z, Jirapradittha J, Sirivichayakul C, et al (2017), “Factors associated with mortality outcomes in neonatal septicemia in Srinagarind hospital, Thailand”, Neonat Pediatr Med, 3(131).
ARTICLE INFO
DOI: 10.12699/jfvpulm.12.37.2021.26
Conflict of Interest
Non
Date of manuscript receiving
15/6/2020
Date of publication after correction
15/7/2021
Article citation
Huy Thach Le, Hung Viet Phan, Van Thanh Le, Nguyen Quang Tung Phan. Study clinical, paraclinical features and the outcome of treatment for neonatal infections in early period at Ninh Thuan provincial general hospital. J Func Vent Pulm 2021;37(12):20-25