
 English
English
 French
French
Acute ischemic stroke in patient with miliary tuberculosis: A case report
Accident vasculaire ischémique aigu chez un patient atteint de tuberculose miliaire: À propos un cas
R. Bouchentouf
Lung Disease department, Avicena Military Hospital Marrakech, Morocco
Corresponding author
Dr. Bouchentouf Rachid
Lung Disease department. Avicena Military Hospital.12 Bd Mouqawama Marrakech 40000. Morocco.
E-mail: bouchentouf_rachid@yahoo.fr
DOI: 10.12699/jfvpulm.12.37.2021.63
ABSTRACT
Miliary tuberculosis is a hematogenous dissemination of Mycobacterium Tuberculosis which involves especially lungs, central nervous system and lymph node.
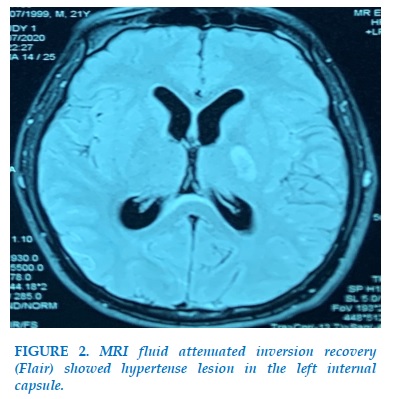
Stroke in tuberculous meningitis (TBM) occurs in 15-57% of patients especially in advance stage and severe illness. We report a 21-year-old man presented with rapid onset confusion and right hemiparesis. he had been recently diagnosed with miliary TB with central nervous system involvement. MRI of brain revealed acute ischemic stroke involving in left internal capsule.
The outcome with antituberculosis treatment and corticosteroids was favorable.
KEYWORDS: Tuberculosis; Miliary; Meningitis; Acute ischemic stroke; Immunocompetent patient
RÉSUMÉ
La tuberculose miliaire est une dissémination hématogène de Mycobacterium Tuberculosis qui touche surtout les poumons, le système nerveux central et les ganglions lymphatiques.
L'AVC (accident vasculaire cérébral) dans la méningite tuberculeuse (TBM) survient chez 15 à 57 % des patients, en particulier à un stade avancé et une maladie grave. Nous rapportons un homme de 21 ans présenté avec une confusion d'apparition rapide et une hémiparésie droite. on lui avait récemment diagnostiqué une tuberculose miliaire avec atteinte du système nerveux central. L'IRM du cerveau a révélé un accident vasculaire cérébral ischémique aigu impliquant la capsule interne gauche.
L'évolution sous traitement antituberculeux et corticoïdes a été favorable.
MOTS CLÉS: Tuberculose; Miliaire; Méningite; AVC ischémique aigu; Patient immunocompétent
INTRODUCTION
Tuberculosis (TB) continues to pose a significant public health problem. In the year 2019, the worldwide estimate of tuberculosis was 10 million new cases and 1.5 million deaths [1]. Tuberculous meningitis (TBM) is the most severe form of extra-pulmonary TB. TBM carries a high mortality rate of 30-40%, including those receiving treatment for TB [2].
The vascular complications in TBM are common and are associated with adverse outcome [3]. The authors describe a case of a man acute stroke secondary to miliary tuberculosis. (lung and cerebral involvement) in immunocompetent patient.
CASE REPORT
A 21-year-old man with no particular pathology history was admitted to a hospital complaining of fever and cough and dyspnea which began a week prior.
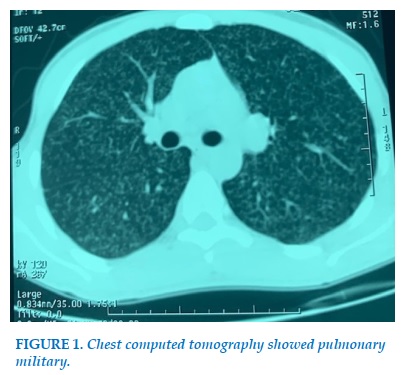
On admission: patient was conscious, polypnea FR 26 cycles/min, tachycardic 120 pbm , SaO2 88%. Pulmonary auscultation found bilateral crackling sounds. The erythrocyte sedimentation rate (ESR) 65 mm 1st hour, hemoglobin 10,5 white blood cells 4500 mm3, neutrophils 65 % lymphocytes 29 % coagulation liver and renal functional tests were normal. A chest radiograph depicted micronodular shadowing consistent with miliary TB. This finding was confirmed with a chest computed tomography (CT) (Figure 1).
On the same day in the absence of neurologic symptoms cerebrospinal was examined. Analysis of cerebrospinal fluid showed glucose 0,23g/L, protein 3,11g/dL, chlore 96 mmol/l, white cells 150/mm3. GeneXpert was positive in sputum and cerebrospinal fluid.
The diagnosis of miliary tuberculosis with meningitis was established. The serology of VIH was negative. Antituberculosis treatment Rifampicin 600 mg/day, Isoniazid 300 mg/day, ethambutol 1200 mg/day and pyrazinamide 1500 mg/day was started. It was associated with corticosteroids (dexamethasone 4 mg) and oxygen.
Four day after the patient presents hemiparesis in right side, weakness and dysarthria.
Glasgow score was 13/15, TA 125/85 mmHg , and Sa O2 92%.
MRI fluid attenuated inversion recovery (Flair) showed: hyperintense lesion left internal capsule (Figure 2).
The angio-MRI with the sequence time of flight (TOF) showed amputation of distal branches of the middle cerebral artery.
We decided to continue corticosteroids with antituberculosis drugs for 9 months, associated with rehabilitation. The outcome after 2 months was favorable
DISCUSSION
Miliary tuberculosis is a hematogenous dissemination of Mycobacterium Tuberculosis which involves especially lungs, central nervous system and lymph node.
Tuberculous meningitis represents 1% from all type of TB in immunocompetent persons and affect commonly in infants or children [4] .
Stroke in tuberculous meningitis (TBM) occurs in 15-57% of patients especially in advance stage and severe illness. The majority of strokes may be asymptomatic because of being in a silent area, deep coma or associated pathology such as spinal arachnoiditis or tuberculoma [5].
TBM related stroke most commonly manifests with focal weakness such as monoplegia, hemiplegia or quadriplegia [6]. The other neurological manifestations of stroke such as sensory impairment, ataxia, seizures, movement disorders, cranial nerve palsy, aphasia, apraxia and hypothalamic disturbances depend on the location of infarctions. The majority of the infarcts are seen in the basal ganglia and internal capsule related to the encasement of the basal perforating arteries, particularly the origin of the lenticulostriate arteries [5].
Cerebral infarction occurs due to involvement of the vessel wall by the inflammatory exudate leading to panarteritis with secondary thrombosis and occlusion [7]. Rarely aneurismal dilatation, ruptured mycotic aneurysm, granulomatous septic embolism has also been suggested [5].
Both CT and angio-MRI detected the ischemic lesion,[8] and diffusion weighted images (DWI) allowed to define the timing of the lesion [9]. Cerebrospinal fluid examination is the cornerstone of TBM diagnosis and the gold standard is the identification of M. tuberculosis in the cerebrospinal fluid (CSF).
TBM patients with stroke have poor clinical outcome. Age, CSF white blood cell and basal meningeal enhancement are risk factors for acute ischemic stroke in young adults with TBM.
All TBM patients should be managed with standard anti-tubercular therapy and supportive treatments. Many studies have shown anti-platelet therapy is beneficial for TBM patients with stroke because of prothrombotic state.
The frequency of stroke and hydrocephalous has been shown to reduce after corticosteroid therapy [10] although in experimental studies inflammatory markers were not affected by corticosteroid [11].
Near Pharmaceutical treatments, the nursing care interventions are very important. The motor and functional rehabilitation permit to prevent muscle atrophy and joint contracture [12].
CONCLUSION
Miliary tuberculosis is a very severe disease with an increased risk of respiratory failure and extensive neurological sequelae and high mortality. Acute stroke may occur in the course of an underlying disease. Miliary Tuberculosis is a risk factor for stroke, timely diagnosis and appropriate management are essential to reducing mortality of this disease.
CONFLICT OF INTEREST
None.
REFERENCE
1. Worl Health Organization. Global Tuberculosis control. WHO report 2019.
2. Foppiano Palacios C, Saleeb PG. Challenges in the diagnosis of tuberculous meningitis.Journal of Clinical Tuberculosis and Other Mycobacterial Diseases 2020, volume 20: 100164.
3. Kalita J, Misra UK, Nair PP. Predictors of stroke and its significance in the outcome of tuberculous meningitis. J Stroke Cerebrovasc Dis 2009; 18: 251-8.
4. Centers for Disease Control and Prevention (2013) Reported Tuberculosis in the United States .US department of Health and Human Service, Atlanta, GA.
5. Misra UK, Kalita J, Maurya PK. Stroke in tuberculous meningitis. J Neurol Sci 2011 15;303(1-2):22-30.
6. Misra UK, Kalita J, Roy AK, Mandal SK, Srivastav M. Role of clinical radiological and neurophysiological changes in predicting the outcome of tuberculous meningitis: an multivariable analysis. J Neurol Neurosurg Psychiatry 2000; 68:300-3.
7. Del Brutto OH. Infections and stroke. In: Ginsberg MD, Bogousslavsky J editors. Cerebrovascular disease. Pathophysiology, diagnosis, and management. Blackwell Science; 1998. p. 1628-46.
8. Lammie GA, Hewlett RH, Schoeman JF, Donald PR. Tuberculous cerebrovascular disease. A review. J Infect. 2009; 59: 156-166.
9. Singh B, Garg RK, Singh MK, Verma R, Malhotra HS, Jain A, Singh R, Kohli N, Phadke RV, Shukla R, Parihar A. Computed tomography angiography in patients with tuberculous meningitis. J Infect. 2012; 64: 565-572.
10. Thwaites GE, Macmullen-Price J, Tran TH, et al. Serial MRI to determine the effect of dexamethasone on the cerebral pathology of tuberculous meningitis: An observational study. Lancet Neurol 2007; 6:230-236.
11. Simmons CP, Thwaites GE, Quyen NT, et al. The clinical benefit of adjunctive dexamethasone in tuberculous meningitis is not associated with measurable attenuation of peripheral or local immune responses. J Immunol 2005; 175:579-590.
12. Dantes E, Hancu A, Iliescu M, Balasa I, Busuioc A, et al. Nursing’s approach and rehabilitation in a severe case of miliary tuberculosis complicated with stroke. ARS Medica Tomitana 2016; 1(2): 56-61.
FIGURES
REFERENCE
1. Worl Health Organization. Global Tuberculosis control. WHO report 2019.
2. Foppiano Palacios C, Saleeb PG. Challenges in the diagnosis of tuberculous meningitis.Journal of Clinical Tuberculosis and Other Mycobacterial Diseases 2020, volume 20: 100164.
3. Kalita J, Misra UK, Nair PP. Predictors of stroke and its significance in the outcome of tuberculous meningitis. J Stroke Cerebrovasc Dis 2009; 18: 251-8.
4. Centers for Disease Control and Prevention (2013) Reported Tuberculosis in the United States .US department of Health and Human Service, Atlanta, GA.
5. Misra UK, Kalita J, Maurya PK. Stroke in tuberculous meningitis. J Neurol Sci 2011 15;303(1-2):22-30.
6. Misra UK, Kalita J, Roy AK, Mandal SK, Srivastav M. Role of clinical radiological and neurophysiological changes in predicting the outcome of tuberculous meningitis: an multivariable analysis. J Neurol Neurosurg Psychiatry 2000; 68:300-3.
7. Del Brutto OH. Infections and stroke. In: Ginsberg MD, Bogousslavsky J editors. Cerebrovascular disease. Pathophysiology, diagnosis, and management. Blackwell Science; 1998. p. 1628-46.
8. Lammie GA, Hewlett RH, Schoeman JF, Donald PR. Tuberculous cerebrovascular disease. A review. J Infect. 2009; 59: 156-166.
9. Singh B, Garg RK, Singh MK, Verma R, Malhotra HS, Jain A, Singh R, Kohli N, Phadke RV, Shukla R, Parihar A. Computed tomography angiography in patients with tuberculous meningitis. J Infect. 2012; 64: 565-572.
10. Thwaites GE, Macmullen-Price J, Tran TH, et al. Serial MRI to determine the effect of dexamethasone on the cerebral pathology of tuberculous meningitis: An observational study. Lancet Neurol 2007; 6:230-236.
11. Simmons CP, Thwaites GE, Quyen NT, et al. The clinical benefit of adjunctive dexamethasone in tuberculous meningitis is not associated with measurable attenuation of peripheral or local immune responses. J Immunol 2005; 175:579-590.
12. Dantes E, Hancu A, Iliescu M, Balasa I, Busuioc A, et al. Nursing’s approach and rehabilitation in a severe case of miliary tuberculosis complicated with stroke. ARS Medica Tomitana 2016; 1(2): 56-61.
ARTICLE INFO
DOI: 10.12699/jfvpulm.12.37.2021.63
Conflict of Interest
Non
Date of manuscript receiving
15/6/2020
Date of publication after correction
15/7/2021
Article citation
Bouchentouf R. Acute ischemic stroke in patient with miliary tuberculosis: A case report. J Func Vent Pulm 2021;37(12):63-65