
 English
English
 French
French
Assessment of spirometry, breath carboxy haemoglobin status in COPD patients & tobacco-smoke quit strategies
Évaluation de la spirometrie, du statut de l'hemoglobine carboxy respiratoire chez les patients BPCO et des strategies pour arreter de fumer du tabac
M. Saifuddin1, M. Hidayath Hussain2
1 : Department of Pulmonary Medicine. Mahavir Institute of Medical Sciences.Vikarabad, Telangana
2 : Department Of Pulmonary Medicine. Shadan Institute of Medical Sciences. Hyderabad
Corresponding author
Dr. Mohammed HIDAYATH HUSSAIN
Department Of Pulmonary Medicine. Shadan Institute of Medical Sciences. Hyderabad.
E-mail: husseink30@yahoo.com
ABSTRACT
Background. More than 5 million of those deaths are the result of direct tobacco use while more than 6,00,000 are the result of non-smokers being exposed to second-hand smoke. Nearly 80% of the world's 1 billion smokers live in low-and middle-income countries.
Objective. The aim of this study was to assess strategies of anti smoking by personal, electronic, spirometric and smoke analyzer, motivational methods.
Methods. All the subjects were administered a questionnaire about tobacco habit details, Spirometry and Carbon Monoxide monitor were used to assess breath carboxyl hemoglobin at regular intervals to motivate and check compliance with anti tobacco strategy. The four parameters from (Spirometry, Smoke Analyser, 6 Minute Walk Test, Reminder Via Electronic Communication) were performed at regular intervals (baseline, 2nd, 3rd, 6th, 9th and at 12th month). Data were presented in the form of statistical Tables and charts. SPSS software version 20 was used for statistical analysis.
Results. Significant improvement was documented in FEV1, 6MWT and Breath COHb from the 3rd month onwards. The quit rate of 40% was achieved at the end of 3 months but 25 of them were lost to follow up and did not respond. 15% honored their consent and commitment and were followed for 1 year. This group demonstrated a successful total quit i.e. 15% and a highly significant improvement in COHb% and 6MWT. FEV1 however showed a minimal significant effect at 12 months.
Conclusion. The study proves that combination pack of strategies to stop smoking among chronic smokers is likely to be successful provided the health personnel involved are fastidious in their implementation. Further work is required in this area in the developing countries to improvise and sustain at a public health framework.
KEYWORDS: Tobacco-smoke; COPD; spirometry; carboxyl hemoglobin.
RÉSUMÉ
Introduction. Plus de 5 millions de ces décès sont le résultat de l'usage direct du tabac tandis que plus de 6 000 000 sont le résultat de l'exposition de non-fumeurs à la fumée secondaire. Près de 80% du milliard de fumeurs dans le monde vivent dans des pays à revenu faible ou intermédiaire.
Objectif. Le but de cette étude était d'évaluer les stratégies de lutte contre le tabagisme par des méthodes de motivation personnelles, électroniques, spirométriques et de fumée.
Méthodes. Tous les sujets ont reçu un questionnaire sur les détails des habitudes tabagiques, une spirométrie et un moniteur de monoxyde de carbone ont été utilisés pour évaluer la respiration carboxyle hémoglobine à intervalles réguliers pour motiver et vérifier la conformité avec la stratégie anti-tabac. Les quatre paramètres de (spirométrie, analyseur de fumée, test de marche de 6 minutes, rappel par communication électronique) ont été effectués à intervalles réguliers (ligne de base, 2e, 3e, 6e, 9e et 12e mois). Les données ont été présentées sous forme de tableaux et graphiques statistiques. La version 20 du logiciel SPSS a été utilisée pour l'analyse statistique.
Résultats. Une amélioration significative a été documentée dans FEV1, 6MWT et Breath COHb à partir du 3ème mois. Le taux d'abandon de 40% a été atteint au bout de 3 mois mais 25 d'entre eux ont été perdus de vue et n'ont pas répondu. 15% ont honoré leur consentement et leur engagement et ont été suivis pendant 1 an. Ce groupe a démontré un abandon total réussi, c'est-à-dire 15% et une amélioration très significative du COHb% et du 6MWT. Le FEV1 a cependant montré un effet significatif minimal à 12 mois.
Conclusion. L'étude prouve qu'un ensemble combiné de stratégies pour arrêter de fumer chez les fumeurs chroniques est susceptible de réussir à condition que le personnel de santé impliqué soit exigeant dans leur mise en œuvre. Des travaux supplémentaires sont nécessaires dans ce domaine dans les pays en développement pour improviser et maintenir un cadre de santé publique.
MOTS CLÉS: Fumée du tabac; BPCO; spirométrie; carboxyle d'hémoglobine
INTRODUCTION
Tobacco is the major cause of death during productive years of their life. The overall untimely deaths produced by tobacco during the last century has been projected about 100 million [1]. Globally, tobacco as a risk factor causes 4.1% of the total burden of disability (WHO, 2002c). It has been estimated that there are 1.1 billion smokers worldwide and 182 million (16.6%) of them live in India [1-4]. It has been predicted by the World Health Organization (WHO) that more than 500 million people alive today will be killed by tobacco by 2030 and tobacco consumption will become the single leading cause of death [5]. India is home to the world's second largest number of tobacco users. Tobacco household survey 2010 covered 99%of Indian population of which 275 million were tobacco users, 111 million will smoke, 206 will chew or both. Due to tobacco smoking habit there will be persistent reduction in FEV1 and FEV1/FVC; these are the characteristic physiological abnormalities of COPD. The reduced FEV1 is not reversible with inhaled bronchodilators, although improvements up .to 15% are common. On average, expiratory air flow decrease twice as fast in smokers (40ml/yr) than non-smokers (20ml/yr) [6]. The smoking of tobacco, particularly as cigarettes, results in increased breath COHb% (carboxy hemoglobin) levels. Whereas COHb concentrations of 5% are rarely found in nonsmokers, concentrations of 5–15% are often found in smokers [7]. In smoking cessation programme ,the measurement of FEV1 by Spirometry and COHb by smoke analyser in expired air may be useful in showing smokers the level of FEV1 and COHb in their exhaled air which decreases overtime after cessation of smoking [8]. The present study is undertaken to study the assessment of Spirometry, COHb in COPD patients and tobacco smoke quit strategies.
METHODS
Place of study. The present study was conducted in a highly polluted urban zone of Langerhouse near the institute (Shadan Institute Of Medical Sciences, Hyderabad, Telanagana).
Type of study. This was a pilot study.
Sample collection. Sample Size : 100 subjects.
Sampling methods. Consecutive sampling.
Inclusion criteria. 100 male smokers who were roadside vendors and shopkeepers were selected for the study.
Statistical methods. Data were presented in the form of statistical Tables and charts. SPSS software version 20 was used for statistical analysis .
Ethical approval. Approval was taken from the Institutional Ethics Committee prior to commencement of the study
RESULTS
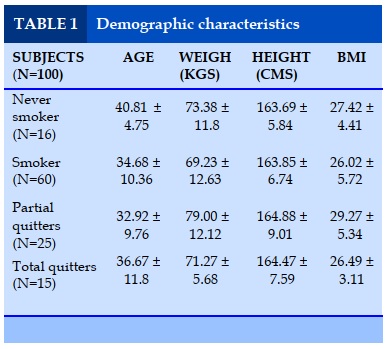
Demographic characteristics (Table 1)
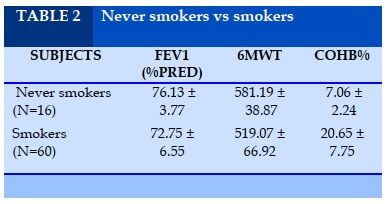
The demographic characteristic of age, height, weight and BMI did not show statistically significant difference between never smoker v/s smoker. (Table 2)
The difference in the 6MWT and COHb% between Never-Smokers and Smokers was highly significant (p<0.0001). No difference was observed in the two groups with reference to FEV1.
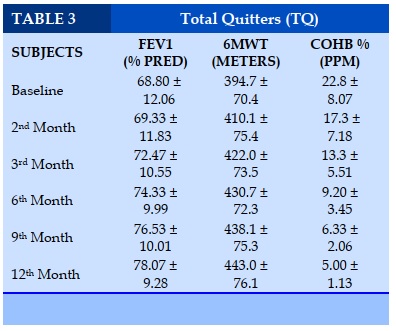
Total quitters (TQ) (Table 3)
Significant improvement was observed in FEV1 in the 12th month versus the initial value (p<0.02). Significant improvement was observed in 6MWT at 3rd,6th,9th,12th month compared to the initial value (p<0.0001). The COHb% demonstrated highly significant reduction at the 3rd,6th,9th,and 12th month compared with the initial value (p<0.0001).
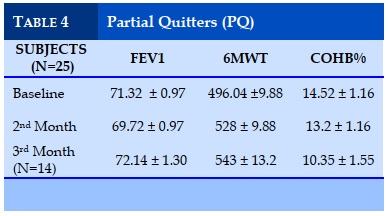
Partial quitters (PQ) (Table 4)
The partial quitter group demonstrated significant improvement in6MWT in the 3rd month (p=0.01) . FEV1 and CoHb did not show statistically significant difference over 3 months.
DISCUSSION
In our study 100 male smokers who are roadside vendors and shopkeepers were selected from a highly polluted area of Langerhouse, and followed up for 1 year. Out of 100 subjects, 40 followed up to 1 year and 60 lost to follow up. Out of 40 subjects 25 are partial quitters who followed up to 3months and 15 subjects are total quitters (TQ). The following parameters Spirometry (FEV1), 6 MWT, COHb% were performed at an interval of 0 ,2nd ,3rd ,6th ,9th ,12th month. In our study, FEV1 among total quitters had significant improvement at 12th month compared to the baseline (p<0.001). The study of Scanlon PD et.al [9]3,926 smokers with mild-to-moderate airway obstruction were randomized to smoking cessation groups or to a nonintervention group. Participants who stopped smoking experienced an improvement in FEV1 in the year after quitting (an average of 47 ml or 2%). The subsequent rate of decline in FEV1 among sustained quitters was half the rate among continuing smokers, 31 +/- 48 versus 62 +/- 55 mL (mean +/- SD), comparable to that of never-smokers. They came to a conclusion that smokers with airflow obstruction benefit from quitting despite previous heavy smoking, advanced age and poor baseline lung function. In the study of Pezzuto A et .al [10] ,, a total of 181 current smokers were prospectively enrolled. All subjects were given 3 months of varenicline plus nicotine-replacement therapy combined with basic counseling. Subjects were sorted into two subgroups after 3 months: quitters and reducers. 30% of their subjects demonstrated severe obstruction. The most significant improvements were obtained in quitters: carboxyl hemoglobin was reduced by 1.06%, the average expiratory flow between 25 and 75% of vital capacity increased by 16% from predicted, mean serum CEA level decreased by 1.83 ng/ml and FEV1 increased by 2.57% from predicted. Subjects with severe obstruction were more compliant to the cessation strategy. Compared to Pezzuto et al study [10] we had only 15% of total quitters as we did not use any pharmacological intervention such as varenicline, bupropion, nicotine replacement therapy are not provided free of cost by any governmental or charitable organizations. The usual cost of such therapies is Rs 200-300/day. Therefore none of our patients hailing from the lower socoieconomic status agreed to purchase these medicines for a prolonged period of 3 months to 12 months. In addition to the total quitters, 4 of our smokers regularly used electronic cigarettes but did not comply with our request to undergo Spirometry and breath carboxy Hb even when they were offered these investigations free of charge. They claimed that they reduced their routine cigarette consumption to less than 5 from 1-2 packs a day after shifting to electronic cigarettes. The study of Tashkin DP et.al [11] examined serial changes in spirometry and Clinical COPD Questionnaire (CCQ) scores (measuring respiratory symptoms and health-related quality of life) in COPD participants by smoking status during a smoking cessation trial. In this randomized, double-blind trial, smokers with mild-to-moderate COPD were treated with varenicline 1 mg b.i.d. or placebo for 12 weeks and followed to Week 52.Change from baseline in post-bronchodilator FEV(1) was significantly improved in continuous abstainers (121.8 mL) vs. continuous smokers (37.9 mL) at Week 12 (P = 0.0069), but not at Weeks 24 or 52. Comparing the above studies (9,10,11) FEV1 shows significant improvement in TQ Vs continuing smokers. Our study has also shown significant improvement in FEV1. In the study of Mantoani et.al [12] 24subjects were assessed at baseline, immediately after completion of the program, and 1 year later for PADL, lung function, 6-min walking distance (6MWD), smoking habits, quality of life, anxiety, and depression. The 5-month program used pedometers and informative booklets as interventions. 20% subjects had quit the smoking habit and improved 6MWT to 694 meters from the baseline of 530 meters. In our study, 6MWD in TQ (N=15) from baseline value of 394+/-70.4(SD) improved to 443.0+/- 76.1(SD) (P=<0.000 )at 12th month. In the study of Mesquita R et.al[13],current smokers and ex-smokers had lower exercise capacity than never smokers on 6MWT. This was a cross sectional study and not a prospective one. In our study COHb% in TQ (N=15) reduced from baseline 22.8+/-8.07 (SD) to 5.00+/-1.13(SD) at 12 month, which shows very significant reduction in COHb% (p=<0.001). An important likely confounder for persistence of higher COHb and failure to return to the lowest possible level of COHb after total quit of smoking is the atmospheric pollution. All the non smoking and smoking subjects in our study hailed from a busy commercial street with a high density of heavy commercial vehicles. They spent 12-14 hours per day in their roadside shops or kiosks. None of the petty shops they ran had an air conditioned environment which could be a barrier to the street vehicular exhaust. The area Langer Houz has been documented as a “high pollutant” area by the Pollution Control Board. The upper limit for respirable particulate matters is 100mcg/cu.mm of air by the Pollution Control Board. The area under study has demonstrated a frightening level of 300mcg/cu.mm by the Pollution Control Board, on par with busy commercial junctions such as Punjagutta. It has previously been shown that COHb is elevated in people using fossil fuels even if they are non smokers. Biomass fuels are considered to be responsible for indoor pollution. The independent effect of vehicular pollution and the additive effect of vehicular pollution plus smoking are difficult to separate in the analysis. In a study of Bednarck M et. al [14] 4494 current smokers were recruited. All subjects were screened by spirometry for signs of airway obstruction. At the time of screening all received simple smoking cessation advice. Spirometry was used as a motivational tool to quit smoking .No pharmacological intervention was done and subjects were followed up for a period of 1 year. Combining Spirometry and exhaled COHb% showed 16.3% smoking cessation rate in subjects with airway obstruction and 12.0% rate in subjects with normal Spirometry (p≤0.0003). In our study, spirometry, 6MWD, COHb%, Text messaging (SMS) and basic counseling showed total quit in 15 subjects who complied with anti tobacco cessation for 1 year. In our study, telephonic counseling and Text messaging shows significantly increased smoking cessation rate 40% at 3 months. However it fell to 15% at 12 months. 25 smokers who were captive to the study for the first 3 months became non responders later.
The study of Curry ST et. al [15], smokers (N = 1,137) were identified through a telephone survey of a random sample. The smoking cessation strategies used were (a) a self-help booklet alone, (b) self-help booklet with computer-generated personalized feedback, and (c) self-help booklet, personalized feedback, and outreach telephone counseling Smoking status was ascertained at 3, 12, and 21 month. Group C showed a high smoking cessation rate of 47% at 3rd month when compared to the two other groups, but not at 12th or 21th month. The study of Michele et.al [16], was done to determine which is the better quit smoking strategy between an SMS (n=76) and Brochure group(n=75). Their study was not supplemented with any other intervention such as physiological parameters or anti smoking cessation drugs. The 3-month sustained abstinence of the subjects was verified by carbon monoxide (CO) readings. There was no statistically significant difference between the groups receiving SMS(11% quit) and Brochure(5% quit).
CONCLUSION
The study concludes that a total quit rate of 15% could be achieved in this cohort hailing from lower socioeconomic status and busy commercial activity in an urban area of Hyderabad. To the best of our knowledge, this is perhaps the only study using combination of the above said strategies in quit smoking program in our country. Though the total quit rate has been small at 15%, it reflects the possibilities for better success with improvisation of strategies and strict adherence to them at a public health program level which deserves further work to validate.
CONFLICT OF INTEREST
Non.
REFERENCES
1. Reddy KS, Gupta PC, editors. Report on Tobacco Control in India. New Delhi: Ministry of Health and Family Welfare; 2004.
2. Prevention of Mental Disorders - World Health Organization.Available from: http://www.who.int/mental_health/./prevention_of_mental_disorders_sr.pdf. [Last cited on 2014 Dec 27].
3. Tobacco Control and Mobile Health, a New Initiative. Available from: http://www.who.int/tobacco/mhealth/mhealth_new_initiative. pdf. [Last cited on 2014 Dec 19].
4. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century- the approach of the WHO Global Oral Health Programme. Available from:http://www.who.int/oral_health/media/en/orh_report03_en.pdf.[Lastcitedon2014 Jun16].
5. Wyne AH, Chohan AN, Al-Moneef MM, Al-Saad AS. Attitudes of general dentists about smoking cessation and prevention in child and adolescent patients in Riyadh, Saudi Arabia. J Contemp Dent Pract 2006;7:35-43.
6. Kohansan R,martinez-camblor P, Agusti A, et al. The natural chronic airflow obstruction revisited:an analysis of Framingham offspring cohort, Am J Respir crit Care Med.2009 Jul 1;180(1):3-10.
7. Russell MA, Cole PV, Brown E. Absorption by non-smokers of carbon monoxide from room air polluted by tobacco smoke. Lancet 1973; 17: 576–579.
8. Jarvis M, Belcher M, Vessey C,Hutchinson D. Low cost carbon monoxide monitors in smoking assessment. Thorax 1986, 41, 886–887.
9. Scanlon PD, Connett JE, Waller LA, Altose MD, Bailey WC, Buist AS, Tashkin DP; Lung Health Study Research Group.Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease. The Lung Health Study.Am J Respir Crit Care Med.2000 Feb;161(2 Pt 1):381-9.
10. Pezzuto A, Spoto C, Vincenzi B, Tonini G.Short-term effectiveness of smoking-cessation treatment on respiratory function and CEA level. J Comp Eff Res.2013 May;2(3):335-43.
11. Tashkin DP1, Rennard S, Taylor Hays J, Lawrence D, Marton JP, Lee TC. Lung function and respiratory symptoms in a 1-year randomized smoking cessation trial of varenicline in COPD patients. Respir Med.2011 Nov;105(11):1682-90.
12. Mantoani LC, Furlanetto KC, Kovelis D, Proença M, Zabatiero J, Bisca G, Morita A, Pitta F Lung function and respiratory symptoms in a 1-year randomized smoking cessation trial of varenicline in COPD patients. Chest.2014 Dec;146(6):1627-32.
13. Mesquita R, Gonçalves CG, Hayashi D, Costa Vde S, Teixeira Dde C, de Freitas ER, Felcar JM, Pitta F, Molari M, Probst VS.Smoking status and its relationship with exercise capacity, physical activity in daily life and quality of life in physically independent, elderly individuals. Physiotherapy.2015 Mar;101(1):55-61.
14. Bednarek M, Gorecka D, Wielgomas J, Czajkowska-Malinowska M, Regula J, Mieszko-Filipczyk G, Jasionowicz M, Bijata-Bronisz R, Lempicka-Jastrzebska M,Czajkowski M, Przybylski G, Zielinski J Smokers with airway obstruction are more likely to quit smoking. Thorax.2006 Oct;61(10):869-73. Epub 2006 Jun 29.
15. Curry SJ, McBride C, Grothaus LC, Louie D, Wagner EH. A randomized trial of self-help materials, personalized feedback, and telephone counseling with nonvolunteer smokers. J Consult Clin Psychol 1995 Dec;63(6):1005-1014.
16. Michele Ybarra, PhD;A Tülay Bağcı Bosi, PhD;Josephine Korchmaros, PhD;Salih Emri, MD A Text Messaging-Based Smoking Cessation Program for Adult Smokers: Randomized Controlled Trial. Journal of Med Internet Research, Nov vol.14 ,no.6(2012).
TABLES
REFERENCES
1. Reddy KS, Gupta PC, editors. Report on Tobacco Control in India. New Delhi: Ministry of Health and Family Welfare; 2004.
2. Prevention of Mental Disorders - World Health Organization.Available from: http://www.who.int/mental_health/./prevention_of_mental_disorders_sr.pdf. [Last cited on 2014 Dec 27].
3. Tobacco Control and Mobile Health, a New Initiative. Available from: http://www.who.int/tobacco/mhealth/mhealth_new_initiative. pdf. [Last cited on 2014 Dec 19].
4. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century- the approach of the WHO Global Oral Health Programme. Available from:http://www.who.int/oral_health/media/en/orh_report03_en.pdf.[Lastcitedon2014 Jun16].
5. Wyne AH, Chohan AN, Al-Moneef MM, Al-Saad AS. Attitudes of general dentists about smoking cessation and prevention in child and adolescent patients in Riyadh, Saudi Arabia. J Contemp Dent Pract 2006;7:35-43.
6. Kohansan R,martinez-camblor P, Agusti A, et al. The natural chronic airflow obstruction revisited:an analysis of Framingham offspring cohort, Am J Respir crit Care Med.2009 Jul 1;180(1):3-10.
7. Russell MA, Cole PV, Brown E. Absorption by non-smokers of carbon monoxide from room air polluted by tobacco smoke. Lancet 1973; 17: 576–579.
8. Jarvis M, Belcher M, Vessey C,Hutchinson D. Low cost carbon monoxide monitors in smoking assessment. Thorax 1986, 41, 886–887.
9. Scanlon PD, Connett JE, Waller LA, Altose MD, Bailey WC, Buist AS, Tashkin DP; Lung Health Study Research Group.Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease. The Lung Health Study.Am J Respir Crit Care Med.2000 Feb;161(2 Pt 1):381-9.
10. Pezzuto A, Spoto C, Vincenzi B, Tonini G.Short-term effectiveness of smoking-cessation treatment on respiratory function and CEA level. J Comp Eff Res.2013 May;2(3):335-43.
11. Tashkin DP1, Rennard S, Taylor Hays J, Lawrence D, Marton JP, Lee TC. Lung function and respiratory symptoms in a 1-year randomized smoking cessation trial of varenicline in COPD patients. Respir Med.2011 Nov;105(11):1682-90.
12. Mantoani LC, Furlanetto KC, Kovelis D, Proença M, Zabatiero J, Bisca G, Morita A, Pitta F Lung function and respiratory symptoms in a 1-year randomized smoking cessation trial of varenicline in COPD patients. Chest.2014 Dec;146(6):1627-32.
13. Mesquita R, Gonçalves CG, Hayashi D, Costa Vde S, Teixeira Dde C, de Freitas ER, Felcar JM, Pitta F, Molari M, Probst VS.Smoking status and its relationship with exercise capacity, physical activity in daily life and quality of life in physically independent, elderly individuals. Physiotherapy.2015 Mar;101(1):55-61.
14. Bednarek M, Gorecka D, Wielgomas J, Czajkowska-Malinowska M, Regula J, Mieszko-Filipczyk G, Jasionowicz M, Bijata-Bronisz R, Lempicka-Jastrzebska M,Czajkowski M, Przybylski G, Zielinski J Smokers with airway obstruction are more likely to quit smoking. Thorax.2006 Oct;61(10):869-73. Epub 2006 Jun 29.
15. Curry SJ, McBride C, Grothaus LC, Louie D, Wagner EH. A randomized trial of self-help materials, personalized feedback, and telephone counseling with nonvolunteer smokers. J Consult Clin Psychol 1995 Dec;63(6):1005-1014.
16. Michele Ybarra, PhD;A Tülay Bağcı Bosi, PhD;Josephine Korchmaros, PhD;Salih Emri, MD A Text Messaging-Based Smoking Cessation Program for Adult Smokers: Randomized Controlled Trial. Journal of Med Internet Research, Nov vol.14 ,no.6(2012).
ARTICLE INFO DOI: 10.12699/jfvpulm.11.33.2020.7 Conflict of Interest