
 English
English
 French
French
Study on the correlation between excessive daytime sleepiness and obstructive sleep apnea
Étude de correlation entre la somnolence excessive diurne et des apnée obstructive du sommeil
K. Dang Thi Mai1, T. Dang Vu1, N. Tran Van1, V. Le Thuong1, H. Vu1, S Duong-Quy2,3
1 : Respiratory Department of Cho Ray Hospital. HCM city, Vietnam
2 : Lam Dong Medical College. Lam Dong, Da Lat, Vietnam
3 : Penn State Medical College. USA
Corresponding author
Dang Thi Mai Khue
Respiratory Department of Cho Ray Hospital HCM city. Vietnam
E-mail: maikhuemd@gmail.com
ABSTRACT
Introduction. The aims of this study were to find out the prevalence of excessive daytime sleepiness (EDS) in patients with OSA and to investigate its correlations with respiratory polygraphy variables.
Method. This cross-sectional analytical study was conducted on 164 subjects, comprising 23 cases of “non-OSA” and 141 cases with OSA. Overnight respiratory polygraphy was done in all the Subjects. Prevalence of EDS were assessed and compared between the two groups.
Results. Prevalence of EDS was significantly higher (36.9%) in patients with OSA than in subjects without OSA (4.3%). Out of 53(36,9%) OSA patients with EDS, 4 (7.7%) had mild OSA, 9 (17.3%) had moderate OSA, and 39 (75%) had severe OSA. Increasing severity of OSA was associated of ESS.
Conclusion. EDS is correlated with the severity of OSA. More severe patients are characterized by higher ESS score, higher BMI, and progressive worsening of nocturnal hypoxemia. Nocturnal hypoxemia is a major determinant of EDS in Vietnamese OSA patients.
KEYWORDS: Obstructive sleep apnea; Epworth Sleepiness Scale; Respiratory polygraphy.
RÉSUMÉ
Objectifs. Les objectifs de cette étude étaient de découvrir la prévalence de la somnolence excessive diurne (SED) chez les patients atteints d'AOS et d'étudier ses corrélations avec les variables de la polygraphie respiratoire.
Méthode. Cette étude analytique transversale a été menée sur 164 sujets, dont 23 cas de «non-AOS» et 141 cas avec AOS. Une polygraphie respiratoire nocturne a été réalisée chez tous les Sujets. La prévalence de SED a été évaluée et comparée entre les deux groupes.
Résultat. La prévalence de SDE était significativement plus élevée (36,9%) chez les patients avec AOS que chez les sujets sans AOS (4,3%). Sur 53 (36,9%) patients souffrant d'AOS avec SDE, 4 (7,7%) avaient une AOS légère, 9 (17,3%) une AOS modérée et 39 (75%) une AOS sévère. La sévérité croissante de l'AOS était associée à SDE.
Conclusion. SDE est corrélé avec la gravité de l'AOS. Les patients plus sévères se caractérisent par un score SDE plus élevé, un IMC (index de masse corporelle) plus élevé et une aggravation progressive de l'hypoxémie nocturne. L'hypoxémie nocturne est un déterminant majeur de l'EDS chez les patients vietnamiens souffrant d'AOS.
MOTS CLÉS: Apnée obstructive du sommeil; Échelle de somnolence d'Epworth; Polygraphie respiratoire.
INTRODUCTION
Obstructive sleep apnea (OSA) is a common disease with an incidence of up to 8.5% in Vietnamese [2]. OSA is characterized by repeated shortness of sleep or shortness of breath caused by collapse of the upper airway during sleep, resulting in fragmented sleep and intermittent hypoxemia, which is an influencing factor. to symptoms of excessive drowsiness in these patients [15]. The Epworth scale (ESS) has been developed since 1991 to quantify the degree of daytime sleepiness and is often used to evaluate patients with OSA or sleep-related illnesses [6]. Excessive drowsiness can increase the risk of traffic accidents, impaired social or professional activities and reduce the quality of life [9] and [10]. Excessive drowsiness is one of the symptoms that helps identify OSA. The prevalence of excessive sleep during the previous study was 87.2% [14]. However, there was also a study that did not find an association with excessive sleepiness and a decrease in apnea (AHI) [1,5,12]. So far, excessive sleepiness is not always a symptom in OSA patients.
Therefore, we conducted a study to investigate the excessive sleepiness rate of OSA patients at Cho Ray Hospital and its correlation with the variables of multiple respiratory signs.
METHODS
The study was carried out in the respiratory department at Cho Ray Hospital and took samples from 2017-2019, including 2 groups of 23 non-OSA patients and 141 patients with OSA.
Selection criteria: Adult patients come to measure multiple respiratory regimens at the respiratory department of Cho Ray Hospital and complete the full ESS question.
Exclusion criteria: Patients did not agree to participate in the study.
Research progress: The study complies with the Helsinki declaration. All patients in the study were explained and signed to participate in the study. Afterwards, all patients were measured for multi-night respiration at the Respiratory Department of Cho Ray Hospital, including electrodes: Nasal electrodes, breast cavity, posture, abdominal waistband, oxygen saturation and heart rate.
The recorded parameters of the multi-respiratory results include: apnea, apnea, apnea (AHI), SpO2 through CIDELEC 2.0 software and re-read by standard compliance researcher of AASM (American Academy of Sleep Medicine) 2012.
The Apnea-Hypopnea Index (AHI) helps assess OSA severity including: non-OSA with AHI <5 times / hour, 5-14 times /hour: light; 15-29 times /hour: average; ≥ 30 times /hour: severe.
In the description of the study population characteristics, the identification variables and the order are presented as the number of objects (n) and the percentage; Continuous variables are presented as mean, median and standard deviation (± SD - standard deviation). If the distribution of these variables is standard, we choose Student t-test to compare the average between the two groups and the ANOVA test to compare the average of 3 or more groups; If the distribution is not normal, we use a non-parametric test to compare the median Mann-Whitney U test or Kruskal Wallis test for 2 groups or from 3 comparison groups or more.
RESULTS
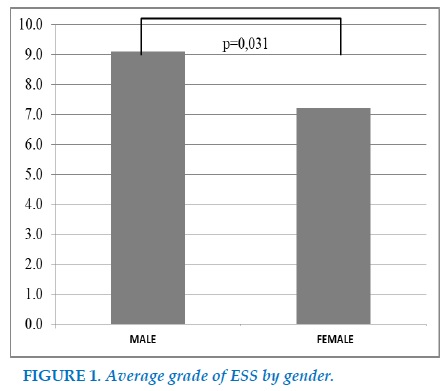
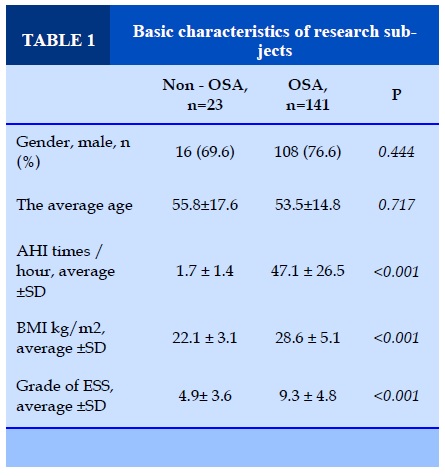
In our study, 164 subjects included; 124 males and 40 females; 23 (16 men) patients were controls and 141 (108 men) patients were OSA. The gender distribution in the two groups is similar. Basic characteristics of the study subjects are described in Table 1.
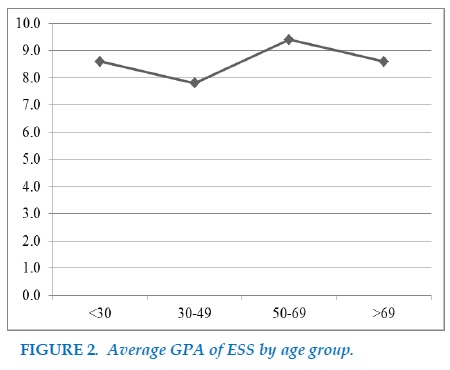
Among the research cases, 7 (4%) have the age group <30; 30-50 years: 59 (36%); 50-70 years old: 70 (43%); ≥ 70 years: 26 (16%). The mean age of the control group 55.8 ± 17.6, of the OSA group: 53.5 ± 14.8, there was no significant difference.
In particular, in the age group 50-70, the OSA group was significantly higher than the control group (P <0.001).
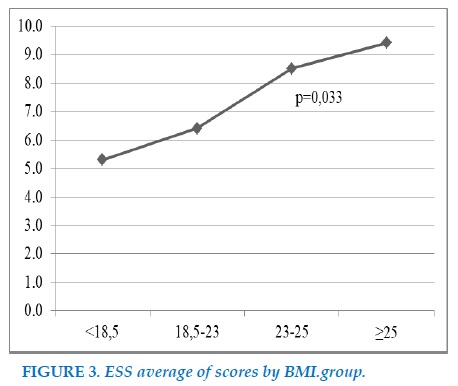
Increased sleepiness with gender and age group
Are presented in Figure 1, 2, 3
There were 141 patients with 4 (2.4%) had BMI <18.5 kg /m2, 22 (13.4%) had BMI from 18.5-23 kg /m2, 27 (16.5%) had BMI from 23-25 kg /m2 and 111 (67.7%) with BMI ≥ 25kg /m2.
The ESS value reaches excessive sleepiness when the ESS> 10 points. The study showed that the proportion of patients with excessive drowsiness in the "non-OSA" group (4.3%, n = 1) was lower than the OSA group (36.9%, n = 52) was statistically significant (P = 0.002). Among OSA patients with excessive drowsiness, there were 4 (7.5%) mild OSA, 9 (17%) average OSA, 39 (73.5%) severe OSA.
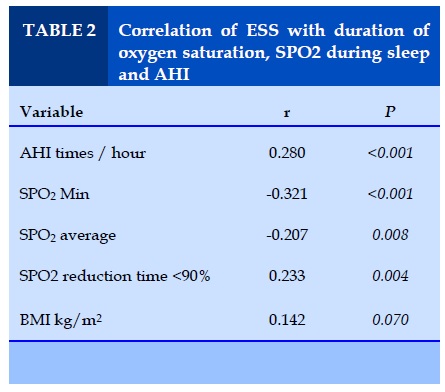
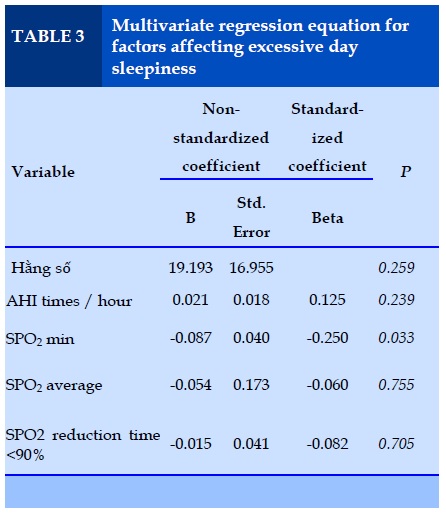
In our study, ESS was positively correlated with AHI, SpO2 reduction time <90% in case and inversely correlated with lowest SpO2 (oxygen saturation) and average SPO2 during sleep.
When included in the multivariate regression equation, the lowest SPO2 during sleep was an independent factor affecting the patient's daily drowsiness. Table 2, 3.
DISCUSSION
Our study shows that OSA weight, sleep oxygen saturation and duration of oxygen saturation are correlated with daily sleepiness. Meanwhile, the average ESS was different between BMI groups but no correlation was found between BMI and ESS. Our study did not show the mean difference in ESS among age groups, while Joel Ci Goh's study showed that young ESSs were higher and correlated with ESS (r = -0.148, P <0.001). [4] or Jing Feng's research has a correlation r = 0.182, p <0.001) [3]. Seung Ju Lee's study had no correlation between age and ESS [8].
ESS is a set of easy-to-use screening questions and basic physicians can use to assess patients and specialists can be used to monitor and evaluate OSA patients. However, the results of evaluating the daily drowsiness rate by ESS differed from the studies. In the Wisconsin Sleep Cohort Study [16], when using a 5-point questionnaire, the questions were asked: waking up not refreshing, time after waking up until falling asleep, falling asleep at night. Day, drowsiness when driving with the answer is regular or daily is considered to be excessive sleepiness. The rate of excessive drowsiness in this study was 22.6% for women and 15.5% for men. While in Seneviratne U's study, this ratio was 87.5% [14]. In our study, the rate of excessive sleepiness in OSA patients was 36.9%. However, in those studies there was no evaluation or correlation of daily drowsiness and multivariate variables. The above studies suggest that ESS does not assess the weight of OSA, it may only relate to date. Up to now, OSA severity has been assessed based on AHI, which is averaged over the number of episodes of apnea stop or apnea [1]. However, only AHI has not yet shown the overall severity of OSA patients such as the lowest oxygen saturation during sleep, the time of oxygen saturation reduction are factors that can affect the consequences of OSA [ 11].
Our research shows the correlation of ESS - a measure of daily sleepiness, one of the consequences of OSA not only for AHI but also for oxygen saturation during sleep and duration of oxygen saturation reduction. Joel Ci Goh's study correlated between ESS and AHI (r = 0.075, P = 0.032), between ESS and lowest SPO2 during sleep (r = -0.071, P = 0.041), time to reduce oxygen saturation ( r = 0.075, P = 0.031) [4]. HSRyo's study had an ESS correlated with AHI (P = 0.027), with the lowest SPO2 during sleep (P = 0.021), but when included in the multivariate regression equation, it was no longer the independent variable affecting. ESS [13]. Seung Ju Lee's study had the lowest correlation between ESS and SPO2 during sleep but no correlation between ESS and AHI [8]. Jing Feng's study correlated between ESS and AHI (r = 0.245, p <0.001) and between ESS and average SPO2 during the night (r = -0.329, p <0.001) [3]. Our study when performing multivariate regression equation of correlation factors with ESS, we found that the lowest SPO2 in true correlation with ESS. This supports the assumption that SPO2 is a determinant of day-to-day sleepiness and should be considered a factor that affects OSA severity. Although the exact mechanism has not been confirmed, it has been hypothesized that excessive sleepiness may lead to impaired brain cognitive function in OSA patients, which is caused by hypoxia. Chronic episodes of sleep [17], [18].
However, this correlation is weak and inconsistent between the studies. In the future we need to do more research with larger color sizes to evaluate this correlation further.
CONCLUSION
ESS was associated with OSA severity although the proportion of patients with excessive daytime drowsiness was not high (39.6%). More research is needed to standardize this questionnaire.
CONFLICT OF INTERREST
Non.
REFERENCES
1. Bixler E. O. et al. (2005), "Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression", J Clin Endocrinol Metab. 90 (8), pp. 4510-4515.
2. Duong-Quy S. et al. (2018), "[Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam]", Rev Mal Respir. 35 (1), pp. 14-24.
3. Feng J. et al. (2012), "Epworth Sleepiness Scale may be an indicator for blood pressure profile and prevalence of coronary artery disease and cerebrovascular disease in patients with obstructive sleep apnea", Sleep Breath. 16 (1), pp. 31-40.
4. Goh J. C. et al. (2018), "Apnoeic and Hypopnoeic Load in Obstructive Sleep Apnoea: Correlation with Epworth Sleepiness Scale", Annals of the Academy of Medicine, Singapore. 47 (6), pp. 216-222.
5. Gottlieb D. J. et al. (1999), "Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study", Am J Respir Crit Care Med. 159 (2), pp. 502-507.
6. Kapur V. K. et al. (2017), "Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline", Journal of clinical sleep medicine: JCSM : official publication of the American Academy of Sleep Medicine. 13 (3), pp. 479-504.
7. Johns M. W. (1991), "A new method for measuring daytime sleepiness: the Epworth sleepiness scale", Sleep. 14 (6), pp. 540-545.
8. Lee S. J. et al. (2012), "The relationship between the Epworth Sleepiness Scale and polysomnographic parameters in obstructive sleep apnea patients", European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 269 (4), pp. 1143-1147.
9. Leger D. (1994), "The cost of sleep-related accidents: a report for the National Commission on Sleep Disorders Research", Sleep. 17 (1), pp. 84-93.
10. Mitler M. M. et al. (1988), "Catastrophes, sleep, and public policy: consensus report", Sleep. 11 (1), pp. 100-109.
11. Muraja-Murro A. et al. (2013), "The severity of individual obstruction events is related to increased mortality rate in severe obstructive sleep apnea", J Sleep Res. 22 (6), pp. 663-669.Johns M. W. (1991), "A new method for measuring daytime sleepiness: the Epworth sleepiness scale", Sleep. 14 (6), pp. 540-545.
12. Roure N. et al. (2008), "Daytime sleepiness and polysomnography in obstructive sleep apnea patients", Sleep Med. 9 (7), pp. 727-731.
13. Ryu H. S. et al. (2016), "Subjective apnoea symptoms are associated with daytime sleepiness in patients with moderate and severe obstructive sleep apnoea: a retrospective study", Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 41 (4), pp. 395-401.
14. Seneviratne U. et al. (2004), "Excessive daytime sleepiness in obstructive sleep apnea: prevalence, severity, and predictors", Sleep Med. 5 (4), pp. 339-343.
15. Uysal A. et al. (2014), "Nocturnal hypoxemia biomarker predicts sleepiness in patients with severe obstructive sleep apnea", Sleep Breath. 18 (1),;77-84.
16. Young T. et al. (1993), "The occurrence of sleep-disordered breathing among middle-aged adults", N Engl J Med. 328 (17), pp. 1230-1235.
17. Zhan G. et al. (2005), "Inducible nitric oxide synthase in long-term intermittent hypoxia: hypersomnolence and brain injury", Am J Respir Crit Care Med. 171 (12), pp. 1414-1420.
18. Zhou L. et al. (2016), "Role of Oxidative Stress in the Neurocognitive Dysfunction of Obstructive Sleep Apnea Syndrome", Oxidative medicine and cellular longevity. 2016, pp. 9626831-9626831.
FIGURES - TABLES
REFERENCES
1. Bixler E. O. et al. (2005), "Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression", J Clin Endocrinol Metab. 90 (8), pp. 4510-4515.
2. Duong-Quy S. et al. (2018), "[Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam]", Rev Mal Respir. 35 (1), pp. 14-24.
3. Feng J. et al. (2012), "Epworth Sleepiness Scale may be an indicator for blood pressure profile and prevalence of coronary artery disease and cerebrovascular disease in patients with obstructive sleep apnea", Sleep Breath. 16 (1), pp. 31-40.
4. Goh J. C. et al. (2018), "Apnoeic and Hypopnoeic Load in Obstructive Sleep Apnoea: Correlation with Epworth Sleepiness Scale", Annals of the Academy of Medicine, Singapore. 47 (6), pp. 216-222.
5. Gottlieb D. J. et al. (1999), "Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study", Am J Respir Crit Care Med. 159 (2), pp. 502-507.
6. Kapur V. K. et al. (2017), "Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline", Journal of clinical sleep medicine: JCSM : official publication of the American Academy of Sleep Medicine. 13 (3), pp. 479-504.
7. Johns M. W. (1991), "A new method for measuring daytime sleepiness: the Epworth sleepiness scale", Sleep. 14 (6), pp. 540-545.
8. Lee S. J. et al. (2012), "The relationship between the Epworth Sleepiness Scale and polysomnographic parameters in obstructive sleep apnea patients", European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 269 (4), pp. 1143-1147.
9. Leger D. (1994), "The cost of sleep-related accidents: a report for the National Commission on Sleep Disorders Research", Sleep. 17 (1), pp. 84-93.
10. Mitler M. M. et al. (1988), "Catastrophes, sleep, and public policy: consensus report", Sleep. 11 (1), pp. 100-109.
11. Muraja-Murro A. et al. (2013), "The severity of individual obstruction events is related to increased mortality rate in severe obstructive sleep apnea", J Sleep Res. 22 (6), pp. 663-669.Johns M. W. (1991), "A new method for measuring daytime sleepiness: the Epworth sleepiness scale", Sleep. 14 (6), pp. 540-545.
12. Roure N. et al. (2008), "Daytime sleepiness and polysomnography in obstructive sleep apnea patients", Sleep Med. 9 (7), pp. 727-731.
13. Ryu H. S. et al. (2016), "Subjective apnoea symptoms are associated with daytime sleepiness in patients with moderate and severe obstructive sleep apnoea: a retrospective study", Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 41 (4), pp. 395-401.
14. Seneviratne U. et al. (2004), "Excessive daytime sleepiness in obstructive sleep apnea: prevalence, severity, and predictors", Sleep Med. 5 (4), pp. 339-343.
15. Uysal A. et al. (2014), "Nocturnal hypoxemia biomarker predicts sleepiness in patients with severe obstructive sleep apnea", Sleep Breath. 18 (1),;77-84.
16. Young T. et al. (1993), "The occurrence of sleep-disordered breathing among middle-aged adults", N Engl J Med. 328 (17), pp. 1230-1235.
17. Zhan G. et al. (2005), "Inducible nitric oxide synthase in long-term intermittent hypoxia: hypersomnolence and brain injury", Am J Respir Crit Care Med. 171 (12), pp. 1414-1420.
18. Zhou L. et al. (2016), "Role of Oxidative Stress in the Neurocognitive Dysfunction of Obstructive Sleep Apnea Syndrome", Oxidative medicine and cellular longevity. 2016, pp. 9626831-9626831.