
 English
English
 French
French
Use of sedatives and muscle relaxants in mechanically ventilated patients and their effect on weaning
Utilisation de sédatifs et de relaxants musculaires chez les patients mécaniquement ventiles et leur effet sur le sevrissement
Mohammed Hidayath Hussain1, Amena Tahseen2, Mansoora Tasneem Sheikh2, Mohamme Saifuddin3.
1: Professor and Head of Department, Department of Pulmonary Medicine, Shadan Institute of Medical Sciences, Hyderabad.
2: 2nd yr post Graduate department of Pulmonology, Shadan Institute of medical Sciences
3: Assistant Professor, Department of Pulmonary Medicine, Mahavir Institute of Medical Sciences. Vikarabad, Telangana
Corresponding author
Dr. Mohammed Saifuddin
Assistant Professor, Department of Pulmonary Medicine
Mahavir Institute of Medical Sciences. Vikarabad, Telangana.
ABSTRACT
Background. Sedatives, analgesics, and paralytic drugs are among the most commonly used medications in the ICU.
Objectives. The present study envisages the role of sedatives and muscle relaxants in patients maintained on mechanical ventilation and their effect on weaning.
Methods. Except the post - operative cases all the cases were intubated in emergency using proper position and Aseptic techniques.
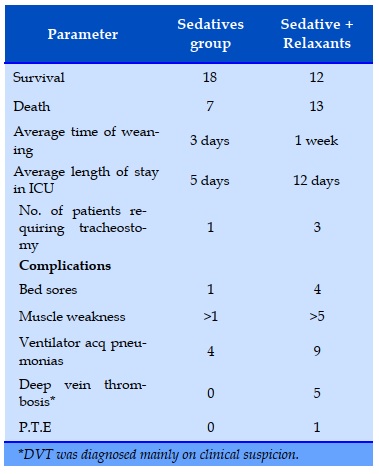
Results. In the sedative group 18 patients survived while in the sedative with relaxant group only 12 patients survived
Conclusion. Patients can be treated by deepening the level of sedation rather than continuously increasing the dose of Neuro-Muscular Blocking Drugs
KEYWORDS: Sedatives; Relaxants; Neuro-muscular blocking drug; Ventilator.
Introduction. Sédatifs, analgésiques et les médicaments paralytiques sont parmi les médicaments les plus couramment utilisés en réanimation
Objectifs. La présente étude envisage le rôle des sédatifs et des myorelaxants chez les patients maintenus sous ventilation mécanique et leur effet sur le sevrage.
Méthodes. À l'exception des cas postopératoires, tous les cas ont été intubés en urgence en utilisant une position appropriée et des techniques aseptiques.
Résultats. Dans le groupe sédatif, 18 patients ont survécu tandis que dans le groupe sédatif avec relaxant, seuls 12 patients ont survécu
Conclusion. Les patients peuvent être traités en approfondissant le niveau de sédation plutôt qu'en augmentant continuellement la dose de médicaments bloquants neuro-musculaires.
MOTS CLÉS: Sédatifs; Relaxants; Médicament neuromusculaire inhibiteur; Ventilateur.
INTRODUCTION
Sedatives. analgesics. and paralytic drugs are among the most commonly used medications in the ICU [1]. Their most important roles include decreasing anxiety and pain (in the case of sedatives and analgesics) and improving tolerance of mechanical ventilation [2,3].
Despite widespread use these agents are often used inappropriately. Reasons include poorly defined therapeutic objectives and inadequately trained medical and nursing staff. Proper use is critical to optimal CCU care [4,5]. An approach to appropriate use of these important drugs is outlined in our study while detailing our experience.
Approach to the Patient
Pain and anxiety are almost universal among the critically ill. Contributing factors include pain from procedures, fear, loss of control, sleep deprivation, and the manifestations of critical illness [6]. Unfortunately, patient discomfort is often under recognized and under treated [7,8]. Agitation may reflect discomfort due to various medical gadgets or underlying disorders that require specific treatment. Potentially life-threatening ones include hypoxia. Hypo glycemia. chest and abdominal pain, CNS infections, and drug or alcohol withdrawal [9].
MATERIALS AND METHODS
Study included 50 cases on mechanical ventilation admitted to the critical care unit, Princess Durru Shehvar Children and General Hospital and Mahavir Hospital and Research Centre, Hyderabad between January 2018 and December 2019
Cases selected were in the age group of 20-60 years
Selection Criteria
Patients maintained on Mechanical Ventilation.
Patients intubated for more than 24 hours
Patients admitted only for the below mentioned disorders:
• ARDS
• Pneumonias
• Left vent failure
• CRF with metabolic acidosis
• Bronchial asthma
• Post-op cases.
Exclusion Criteria
• Patients requiring non-invasive ventilation.
• COPT
• Patients with abnormal liver function tests
Investigations
Following investigations were done in all patients:
• Chest X-Ray
• ABG
• CBP
• Serum Electrolytes
• ECG
• IIIV Screening
• Lung Compliance (Measured on Ventilator)
• Lung Volumes (Measured on Ventilator)
• Bronchoscopy — Cultures for cases of pneumonias.
Methods
Except the post - operative cases all the cases were intubated in emergency using proper position and Aseptic techniques.
Ventilator and settings
All the patients in this study were managed with SIEMENS-SERVO 300 Ventilator. Initial settings after intubation (control mode):
• Tidal Volume: 7-10 ml/kg except in ARDS where 6m1/kg
• Frequency16-18 bpm
• Fi02 0.8% to 1
• Peak Pressure 40 ems of water
• PEEP 5 ems of water
• Min. Volume : 5-10 L/min.
After the initial settings ABG is done and based on the blood gases change in the mode of ventilation and oxygenation was done. Chest X-Ray and ABG were done need based atleast once daily. Patient's were regularly monitored with continuous Sp02. Blood Pressure, ECG monitoring. maintenance of central venous pressure. fluid electrolyte balance and regular suction and chest physiotherapy. No. of days taken to be weaned from mechanical ventilator for each case were recorded.
RESULTS
50 cases were enrolled into the study. age group selected were 20- 60 yrs. Patients were maintained on mechanical ventilation and were given sedatives and muscle relaxants required. Patients were monitored and their hemodynamic status was well maintained. Most of the patients were intubated in emergency and only four cases were taken from electively intubated patients. All the cases were given sedatives as required and relaxants were given only in very restless and agitated cases. No. of days taken for the patients were recorded in both groups and results were recorded.
The following results were seen. Over 50 patients were enrolled into the study. Patients in the sedative groups were treated with IV Midazolam and IV Diazepam sedation was given only as requited and was not on maintenance basis.
DISCUSSION
Routine use of muscle relaxants in the ICU has become much less popular.10 Although they are the agents of choice for achieving muscle relaxation for endotracheal intubation, they have unwanted side effects in critically ill patients that limit their use. 11
One of the most frequent complications occurs with the use of non-depolarizing muscle relaxants in patients with severe respiratory failure due to asthma.12 These patients usually receive corticosteroids for their reactive airway disease, and these agents appear to interact with muscle relaxants to cause a severe form of critical illness called polyneuropathy. This syndrome is characterized by profound peripheral muscle weakness and the appearance of myocyte dropout on muscle biopsy.
Nerve conduction studies are normal. This syndrome may occur within 1-2 days and may take months to resolve. The mechanism is unknown.
Other complications of continuous muscle relaxant use include an increased incidence of ventilator-associated pneumonia, increased incidence of skin pressure ulceration, and the possibility that a patient may be aware and/or in pain. but unable to express discomfort because of the muscle relaxant.
Continuous muscle relaxation should be sought only after intravenous sedatives and analgesics have proven ineffective in facilitating mechanical ventilation. Patients should be monitored for degree of muscle relaxation by using a peripheral nerve stimulator, and the muscle relaxant should be titrated via continuous infusion to maintain the minimum effective degree of relaxation, rather than complete paralysis. However, muscle biopsies and nerve conduction studies were not performed in this study due to financial constraints of the patients.
CONCLUSION
Safety of the long-term administration of Neuro-Muscular Blocking Agents to critically ill patient's remains of great concern. Numerous studies done in this subject clearly show that there is increased incidence of myopathies and neuropathies in critically ill patients. The results of this study highlight the increased incidence of complications that may arise by the use of Neuro-Muscular Blocking Agents. Hence the anxious and agitated patients can be treated by deepening the level of sedation rather than continuously increasing the dose of Neuro-Muscular Blocking Drugs.
CONFLIT OF INTEREST
Non.
REFERENCES
1. Neuro Muscular Blocking Agents and Sedative Drugs -Clinical Uses and toxic effects- Dublin CG-Jr Critical Care Clinics-1991-July 7 (3): 489-506
2. Postal Survey On the long term use of NeuroMuscular Blockade in Intensive Care- Intensive Care
Medicine-I 996- Sept 22(9)-841-843
3. Anesthetics. Sedatives and Paralytics-Understanding their use in the ICU-Aranda M, Hanson-Surgical Clinics of North America-2000-Jane 80(3)-933-942.
4. NMBA'S in the management of respiratory failureIndications, treatment and guidelines-Adam Sapistrien, William Hurford-Critical Care Clinics-Volume 10- Number-4-Oct-1994.
5. lanson-Ftaschen-JH. Brazinsky S, Basile C-Use of sedating drugs and Neuro- Muscular Blocking Drugs in patients requiring Mechanical Ventilation-JAMA-1991- 266: 2870-2876.
6. Cousin.DB: Neuro muscular blockade — should patients be relaxed in ICU-chest- 1992-102-988-989.
7. Gooch IL, Luchezta.MB, etal. Prolonged paralysis after treatment with NMBA'S.- Critical care medicine — 19— 1123-1991.
8. Griffin D, Fairman N, Cousin D, et.ac, Acute myopathy during treatment of status Asthmaticus with steroids and muscle relaxants- chest 102:510- 1992 9. S.Dean, C.M.Lee, J.R.Curtis — Altered neuro muscular disorders in ICU-American journal of respiratory and critical care medicine- oct-1-2003 -168(7):73
10. Ramsay MA, Savege TM, Simpson BR, et al. Controlled sedation with alphaxalone- alphadolone. BMJ 1974; 2:656-659
11. Hansen-Flaschen J, Cowen J, Palomano RC. Beyond the Ramsay scale: need for a validated measure of sedating drug efficacy in the intensive care unit. Crit Care Med 1994; 22:732- 733 imal intravenous dosing strategies for
12. Barr J, Donner A. Opt and analgesics in the intensive care unit. Crit Care Clin sedatives 1995; 11:827847.
TABLE
REFERENCES
1. Neuro Muscular Blocking Agents and Sedative Drugs -Clinical Uses and toxic effects- Dublin CG-Jr Critical Care Clinics-1991-July 7 (3): 489-506
2. Postal Survey On the long term use of NeuroMuscular Blockade in Intensive Care- Intensive Care
Medicine-I 996- Sept 22(9)-841-843
3. Anesthetics. Sedatives and Paralytics-Understanding their use in the ICU-Aranda M, Hanson-Surgical Clinics of North America-2000-Jane 80(3)-933-942.
4. NMBA'S in the management of respiratory failureIndications, treatment and guidelines-Adam Sapistrien, William Hurford-Critical Care Clinics-Volume 10- Number-4-Oct-1994.
5. lanson-Ftaschen-JH. Brazinsky S, Basile C-Use of sedating drugs and Neuro- Muscular Blocking Drugs in patients requiring Mechanical Ventilation-JAMA-1991- 266: 2870-2876.
6. Cousin.DB: Neuro muscular blockade — should patients be relaxed in ICU-chest- 1992-102-988-989.
7. Gooch IL, Luchezta.MB, etal. Prolonged paralysis after treatment with NMBA'S.- Critical care medicine — 19— 1123-1991.
8. Griffin D, Fairman N, Cousin D, et.ac, Acute myopathy during treatment of status Asthmaticus with steroids and muscle relaxants- chest 102:510- 1992 9. S.Dean, C.M.Lee, J.R.Curtis — Altered neuro muscular disorders in ICU-American journal of respiratory and critical care medicine- oct-1-2003 -168(7):73
10. Ramsay MA, Savege TM, Simpson BR, et al. Controlled sedation with alphaxalone- alphadolone. BMJ 1974; 2:656-659
11. Hansen-Flaschen J, Cowen J, Palomano RC. Beyond the Ramsay scale: need for a validated measure of sedating drug efficacy in the intensive care unit. Crit Care Med 1994; 22:732- 733 imal intravenous dosing strategies for
12. Barr J, Donner A. Opt and analgesics in the intensive care unit. Crit Care Clin sedatives 1995; 11:827847.