
 English
English
 French
French
Tracheoesophageal fistula as a complication of tracheostomy
Fistule trachéo-œsophagienne comme complication de la trachéotomie
A. Tahseen, M. Tasneem Sheikh, M. Hidayath Hussain
Department of Pulmonology, Shadan Institute of Medical Sciences. India
Corresponding author
Pr. Dr. Mohammed Hidayath Hussain
Department of Pulmonology. Shadan Institute of Medical Sciences. India
E-mail: drhidayathsims@gmail.com
Acquired tracheoesophageal fistula are commonly due to malignancy.
Benign fistulas are uncommon. Of the non malignant reports of acquired tracheoesophageal fistula, 75% are the results of endotracheal cuff related trauma in patients subjected to prolonged ventilation. Secondary erosion of the tracheal and esophageal walls occur with a 0.3% -3% incidence in mechanically ventilated patients. Tracheostomy doesn’t appear to reduce the risk of developing an acquired tracheoesophageal fistula as a consequence of mechanical ventilation. We present the case of 64 year old male tracheostomised for 20days with increased oral secretions and aspiration of ryle’s tube feeds through tracheostomy tube. On bronchoscopic evaluation found tracheoesophageal fistula.
This report has been presented the case of a patient with tracheostomy developing tracheoesophageal fistula and report an approach in its management.
KEYWORDS: Tracheoesophageal fistula; Tracheostomy.
Les fistules trachéo-œsophagiennes acquises sont généralement dues à une tumeur maligne.
Les fistules bénignes sont rares. Parmi les rapports non malins de fistule trachéo-œsophagienne acquise, 75% sont les résultats de traumatismes liés à la coiffe endotrachéale chez des patients soumis à une ventilation prolongée. Une érosion secondaire des parois trachéale et œsophagienne se produit avec une incidence de 0,3% à 3% chez les patients ventilés mécaniquement. La trachéotomie ne semble pas réduire le risque de développer une fistule trachéo-œsophagienne acquise suite à une ventilation mécanique. Nous présentons le cas d’un homme de 64 ans trachéotomisé pendant 20 jours avec une augmentation des sécrétions orales et une aspiration des tubes de ryle par tube de trachéotomie. Lors de l'évaluation bronchoscopique, une fistule trachéo-œsophagienne a été trouvée.
Ce cas clinique présente d'un patient atteint de trachéotomie développant une fistule trachéo-œsophagienne et rapportons une approche dans sa prise en charge.
MOTS CLÉS: Fistule trachéo-oesophagienne; Trachéotomie.
INTRODUCTION
Acquired tracheoesophageal fistula are most commonly due to malignancy. Benign fistulas are uncommon. Of the non malignant reports of acquired tracheoesophageal fistula , 75% are the results of endotracheal cuff related trauma in patients subjected to prolonged ventilation. Secondary erosion of the tracheal and esophageal walls occur with a 0.3% -3% incidence in mechanically ventilated patients [2]. Tracheostomy doesn’t appear to reduce the risk of developing an acquired tracheoesophageal fistula as a consequence of mechanical ventilation. We present the case of 64 year old male tracheostomized for 20days with increased oral secretions and aspiration of ryle’s tube feeds through tracheostomy tube. On bronchoscopic evaluation found tracheoesophageal fistula.
CASE REPORT
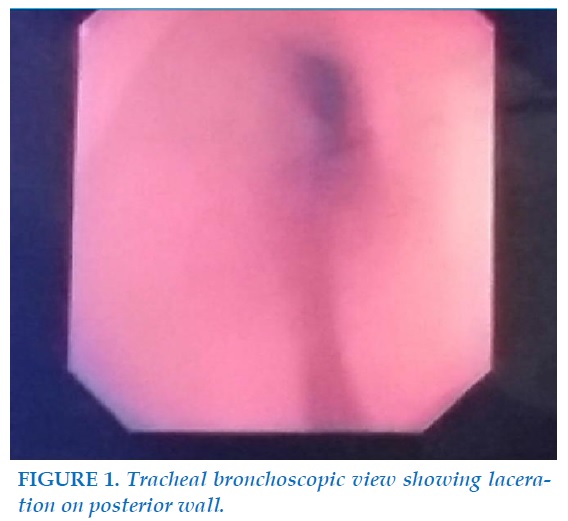
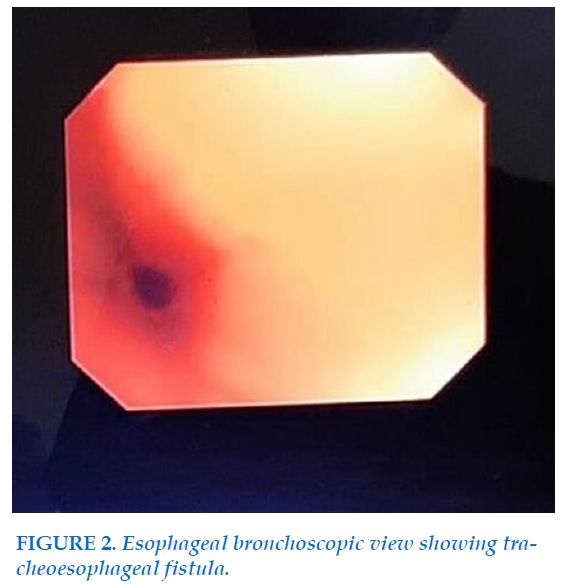
A 64 year old male was transferred to our facility from an outside institution with the diagnosis of cerebellar infarct with basilar artery thrombosis and with tracheostomy done due to aspiration of oral feeding. Tracheostomy was done after failure of endotracheal tube intubation. After a duration of 10 days from the tracheostomy patient was having increased oral secretions and aspiration of the ryle’s feed through the tracheostomy tube and patient was requiring frequent suctioning. On auscultation inspiratory crackles and diminished breath sounds heard at lung bases. Under sedation bronchoscopy performed. Bronchoscope is entered through the nostril reached vocal cords which were edematous and moving equal bilaterally, then entered trachea where increased secretions and a linear laceration seen on the posterior wall of trachea (Figure 1). Esophagus is visualized confirming tracheoesophageal fistula (Figure 2).
DISCUSSION
A tracheoesophageal fistula (TEF) is an epithelialized tract between the esophagus and the trachea. Fistulas can be a result of benign or malignant causes.
Causes of non malignant acquired tracheoesophageal fistula
Blunt or penetrating trauma.
Granulomatous infection.
Previous surgery of trachea and esophagus.
HIV Infection [1,15-18].
Corrosive fluid ingestion.
Poisons and inhalation burns.
Small battery ingestion [6].
Iatrogenic.
Oesophageal stenting.
Oesophageal or tracheal endoscopy.
Transoesophageal echocardiography.
Tracheal tubes and intubation.
Percutaneous tracheostomy [16].
Risk factors predisposing to tracheoesphageal fistula
Excessive motion of the endotracheal tube.
Hypotension.
Diabetes.
Poor nutritional status.
Episodic hypotension.
Restless/awake patients.
Steroid therapy [7].
Poor general state.
Airway infection.
Posterior counter-pressure by nasogastric tubes.
Long-term mechanical ventilation.
Historically, high-pressure tracheostomy cuffs 25-30mmHg were responsible for most fistulas. Since the advent of the high-volume low-pressure cuff, the incidence of cuff-related TEFs has gone down [8,9].
Fistulas are now seen in only 0.5% of patients undergoing a tracheostomy 3,4
Postintubation tracheoesophageal fistula – is a severe complication found in patients that require prolonged mechanical ventilation.
It is induced by ischemia of the posterior tracheal wall caused by the overinflated cuff of the endotracheal or tracheotomy tube that is almost always in contact with a nasogastric tube used for either feeding oral aspirating the gastric content.
Malignant cause
Fistulas can also occur as a result of erosion of tumor from the esophagus into the trachea or from the trachea into the esophagus.
Management and outcomes vary with the etiology of the fistula.
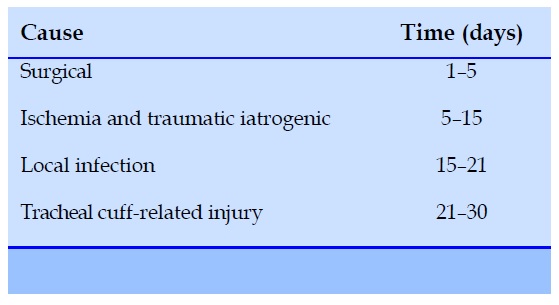
Time course for symptomatic presentation of acquired TOF related to cause.
Clinical features
The most common clinical signs of TEF are coughing while swallowing or drinking purulent bronchitis
Pneumonia.
Dysphagia
An acquired TOF should be considered in any ventilated patient who has unexplained weight loss, recurrent chest infections5 and repeated failures to wean.
Persistent tracheal soiling results in increased secretions on suctioning and subsequent pneumonia.
Positive pressure ventilation can force gas through the patent fistula resulting in gastric dilatation13 and diaphragmatic splinting.
Ono’s sign - refers to the uncontrolled coughing after swallowing, often worse with carbonated drinks.
Other features which should raise suspicions of an acquired TOF are:
History of trauma.
Malignancy.
Ingestion of caustic substances.
Chest pain.
Hemoptysis.
Shortness of breath.
Dysphagia.
Hoarseness.
Pyrexia of unknown origin.
Repeated respiratory tract infections; and pneumonia.
DIAGNOSIS
Chest Xray
Will demonstrate the effects of repeated soiling, fleecy basal infiltrates and the extent of the white-out revealing its severity.
An over-inflated cuff, wider than the tracheal diameter, may suggest a cuff-related TOF.
Endoscopy
Is the best diagnostic method available for awake and asleep patients.
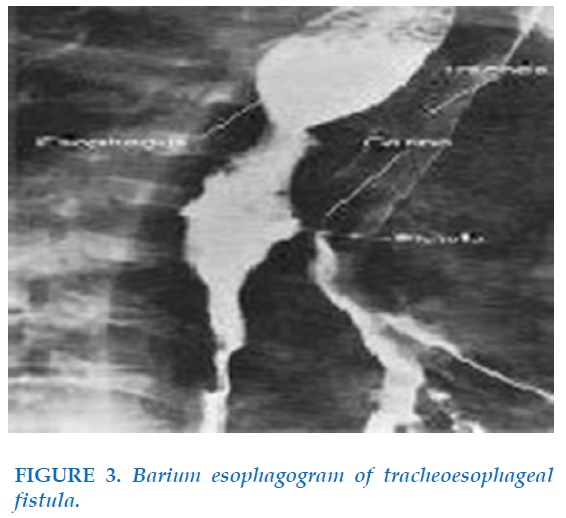
Barium Esophagogram
Helpful to identify laterality and is essential in situations in which an experienced endoscopist is not available (Figure 3).
The radiograph will demonstrate brisk opacification of the esophagus with faint opacification of the airway at and below the level of the fistula.
The absence of barium in the airway above the level of the fistula eliminates the possibility of aspiration as the cause of opacification of the airway.
HRCT has also gained favor in the detection of tracheoesophageal fistulas.
Recent advances have allowed sagittal, coronal, and three-dimensional reconstructions that can help to identify small fistulous tracts [24].
Flexible and rigid bronchoscopy
Identifies the TOF orifice better on the smooth posterior membranous wall and facilitates tissue biopsies. The instillation of methylene blue into the oesophagus can help pin-point the TOF. Bronchoscopy also allows broncho–alveolar lavage, enabling targeted antibiotic therapy and airway clearance2. Accurate identification of the site of the TOF is central to successful definitive management.
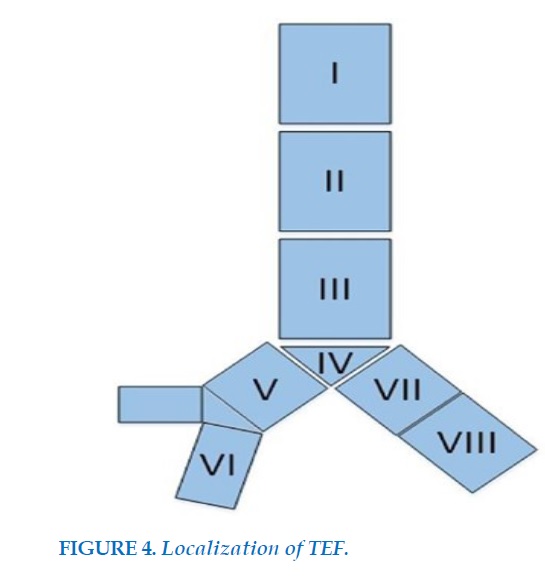
Localization of TEF
For proper localization of TEFs previously Wang and colleagues12 TEF classification system was modeled. The proposed system includes eight zones which classify various fistula locations; Locations I–III were defined the same as that for central airway stenosis. While locations IV–VIII pertaining to the trachea carina and right main, right middle, proximal, and distal bronchi, respectively (Figure 4).
Eight locations of the central airway:
Location I - upper third of the trachea.
Location II - middle third of the trachea.
Location III - lower third of the trachea.
Location IV - trachea carina.
Location V - right main bronchus.
Location VI - right middle bronchus.
Location VII - proximal of left main bronchus.
Location VIII - distal of left main bronchus [12].
Pre operative management
The principles of preoperative management of an acquired TOF are:
To minimize further aspiration, prevent and treat pulmonary infections, provide supportive therapy until definitive surgery [6,10,11].
To prevent tracheal soiling, active methods of protection must be used.
A new endotracheal tube (ETT) or tracheostomy tube should be passed with the cuff lying beyond the lesion.
The bed head should be elevated to prevent further passive regurgitation.
Aggressive pulmonary toileting should be used.
Nasogastric tubes should be removed and replaced with a draining gastrostomy tube to reduce reflux in addition to acid suppression therapy.
In persistent soiling and carinal TOF, there is a case for esophageal diversion.
A gastrostomy is placed for feeding and the oesophagus is divided at the gastro-esophageal junction.
This carries a considerably higher rate of morbidity and mortality.
Esophageal diversion is useful in symptom palliation for malignant cases.
The treatment of a TEF occurs in two stages.
First stage
Preventing further contamination of the lungs.
The patient is kept NPO
A feeding tube (gastrostomy or jejunostomy) is placed.
A course of IV antibiotics is given to help clean up.
the infection that is usually harbored in the lung.
A temporary esophageal stent is placed if the fistula is large and there is evidence of gross contamination.
Protection of the airway may include intubation with placement of the cuff below the fistula to help isolate the distal airway from enteric contamination14.
Airway stents
Covered self-expanding stents Silicone stents
Double stents
Over-the-scope clipping [19,20]
Second stage
Obliterating the fistulous tract and may be done endoscopically or surgically.
Endoscopic ablation
Requires repeated interventions, every 3 to 4 weeks, over a 3-month period during which time the patient remains NPO.
It is a reasonable option in patients with small fistulas or in patients
Too debilitated to undergo an operation.
The application of biologic glues to obliterate a small fistulous tract also may be done.
In most cases, surgical repair is necessary.
Although surgical repair is much more extensive, most patients recover quickly and are able to begin eating within a week of the operation.
Every attempt is made to wean the patient from mechanical ventilation before definitive intervention because postoperative positive-pressure ventilation increases the rate of dehiscence of the repair.
Surgical repair- three stages
The first stage is exposure of the fistulous tract through a cervical or thoracotomy incision.
Stage two is segmental resection of the trachea and primary repair of the esophagus.
Stage three is harvesting an appropriate muscle flap and placing it between the trachea and the esophagus to encourage healing, contain leaks, and prevent future fistulation.
In the case of repair of a postintubation TEF, tracheal resection and primary anastomosis decreases the rate of tracheal stenosis even in the absence of obvious tracheal damage [23].
Other airway fistula treatments include fibrin glue [22], degradable stents, endobronchial one-way umbrella-shaped valves, septal buttons, and transplantation of mesenchymal stem cells.
CONFLICT OF INTEREST
Non.
REFERENCES
1. Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am 2003; 13: 271–89.
2. Couraud L, Ballester ML, Delaisement C. Acquired tracheoesophageal fistula and its management. Semin Thorac Cardiovasc Surg 1998; 8: 392–9.
3. Harley HR. Ulcerative tracheo-oesophageal fistula during treatment by tracheostomy and intermittent positive pressure ventilation. Thorax. 1972;27(3):338- 52.
4. Mathisen DJ, Grillo HC, Wain JC, Hilgenberg AD. Management of acquired nonmalignant trache-oesophageal fistula. Ann Thorac Surg. 1991;52(4):759-65.
5. https://www.sciencedirect.com/science/article/abs/pii/000349759191207C.
6. Berklee R, Das A. Anaesthetic management of ac-quired tracheoesophageal fistula: a brief report. Anesth Analg 2001; 93: 903–5.
7. Macchiarini P, Verhoye JP, Chapelier A, Fadel E, Dart-evelle P.Evaluation and outcome of different surgical techniques for postintubation tracheoesophageal fis-tulas. J Thorac Cardiovasc Surg. 2000;119(2):268-76.
8. Klainer AS, Turndorf H, Maewal H, Allender P. Surface alterations due to endotracheal intubation. Am J Med. 1975;58(5):674-83.
9. Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy. A prospective study of150 critically ill adult patients. Am J Med. 1981;70(1):65-76.
10. Chauhan SS, Long J. Management of tracheoesopha-geal fistula in adults. Curr Treat Options Gastroenter-ol 2004; 7: 31–40.
11. Shah CP, Yeolaker ME, Pardiwala FK. Acquired trache-oesophageal fistula.J Postgrad Med 1994; 40: 83–4.
12. Wang H, Tao M, Zhang N, et al. Airway covered me-tallic stent based on different fistula location and size in malignant tracheoesophageal fistula. Am J Med Sci 2015; 350: 364–368.
13. Sue RD, Susanto I. Long-term complications of artificial airways.Clin Chest Med 2003;24(3):457–471.
14. Horishita T, Junichi O, Kouichiro M. Unique anesthetic management of a patient with a large tracheoesophageal fistula using fibreoptic bronchoscopy.Anesth Analg 2003; 97: 1856.
15. Grillo HC. Surgery of the Trachea and Bronchi. Ac-quired Tracheoesophageal and Bronchoesophageal Fis-tula. London, BC Decker Inc. 2004; 341–56.
16. Trottier SJ, Hazard PB, Sakabu SA, Levine JH, Troop BR, Thompson JA, McNary R. Posterior tracheal wall perfo-rationduring percutaneous dilational tracheostomy: an investigation in to its mechanism and prevention. Chest 1999; 115: 1383–9.
17. Baisi A, Bonavina L, Narne S, Peracchia A. Benign tra-cheoesophageal fistula: results of surgical therapy. Dis Esophagus 1999; 12: 209–11.
18. Ladurner R, Schulz C, Jacob P, Kuper M, Kratt T, Preyer S, Konigsrainer A. Surgical management of an esoph-agotracheal fistula as a severe late complication of re-peated endoscopic stenting treatment. Endoscopy 2007; 39: E341–2.
19. Dogan UB, Akin MS, Yalaki S. Endoscopic closure of tracheoesophageal fistulas with the over-the- scope clip system. J Coll Physicians Surg Pak 2014;24:S193-5.
20. Silon B, Siddiqui AA, Taylor LJ, et al. Endoscopic mana-gement of esophagorespiratory fistulas: a multicenter retrospective study of techniques and outcomes. Dig Dis Sci 2017;62:424-31.
21. Dallemagne B, Weerts J, Markiewicz S, et al: Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc 2006; 20:159-165.
22. Tzifa KT, Maxwell EL, Chait P, et al: Endoscopic treatment of congenital H-type and recurrent tracheoesophageal fistula with electrocautery and histoacryl glue. Int J Pediatr Otorhinolaryngol 2006; 70:925-930.
23. Flum DR, Koepsell T, Heagerty P, et al: The nationwide frequency of major adverse outcomes in antireflux sur-gery and the role of surgeon experience, 1992-1997.J Am Coll Surg 2002; 195:611-618.
24. Cadiere GB, Himpens J, Rajan A, et al: Laparoscopic Nissen fundoplication: Laparoscopic dissection tech-nique and results. Hepatogastroenterology 1997; 44:4-10.
FIGURES - TABLE
REFERENCES
1. Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am 2003; 13: 271–89.
2. Couraud L, Ballester ML, Delaisement C. Acquired tracheoesophageal fistula and its management. Semin Thorac Cardiovasc Surg 1998; 8: 392–9.
3. Harley HR. Ulcerative tracheo-oesophageal fistula during treatment by tracheostomy and intermittent positive pressure ventilation. Thorax. 1972;27(3):338- 52.
4. Mathisen DJ, Grillo HC, Wain JC, Hilgenberg AD. Management of acquired nonmalignant trache-oesophageal fistula. Ann Thorac Surg. 1991;52(4):759-65.
5. https://www.sciencedirect.com/science/article/abs/pii/000349759191207C.
6. Berklee R, Das A. Anaesthetic management of ac-quired tracheoesophageal fistula: a brief report. Anesth Analg 2001; 93: 903–5.
7. Macchiarini P, Verhoye JP, Chapelier A, Fadel E, Dart-evelle P.Evaluation and outcome of different surgical techniques for postintubation tracheoesophageal fis-tulas. J Thorac Cardiovasc Surg. 2000;119(2):268-76.
8. Klainer AS, Turndorf H, Maewal H, Allender P. Surface alterations due to endotracheal intubation. Am J Med. 1975;58(5):674-83.
9. Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy. A prospective study of150 critically ill adult patients. Am J Med. 1981;70(1):65-76.
10. Chauhan SS, Long J. Management of tracheoesopha-geal fistula in adults. Curr Treat Options Gastroenter-ol 2004; 7: 31–40.
11. Shah CP, Yeolaker ME, Pardiwala FK. Acquired trache-oesophageal fistula.J Postgrad Med 1994; 40: 83–4.
12. Wang H, Tao M, Zhang N, et al. Airway covered me-tallic stent based on different fistula location and size in malignant tracheoesophageal fistula. Am J Med Sci 2015; 350: 364–368.
13. Sue RD, Susanto I. Long-term complications of artificial airways.Clin Chest Med 2003;24(3):457–471.
14. Horishita T, Junichi O, Kouichiro M. Unique anesthetic management of a patient with a large tracheoesophageal fistula using fibreoptic bronchoscopy.Anesth Analg 2003; 97: 1856.
15. Grillo HC. Surgery of the Trachea and Bronchi. Ac-quired Tracheoesophageal and Bronchoesophageal Fis-tula. London, BC Decker Inc. 2004; 341–56.
16. Trottier SJ, Hazard PB, Sakabu SA, Levine JH, Troop BR, Thompson JA, McNary R. Posterior tracheal wall perfo-rationduring percutaneous dilational tracheostomy: an investigation in to its mechanism and prevention. Chest 1999; 115: 1383–9.
17. Baisi A, Bonavina L, Narne S, Peracchia A. Benign tra-cheoesophageal fistula: results of surgical therapy. Dis Esophagus 1999; 12: 209–11.
18. Ladurner R, Schulz C, Jacob P, Kuper M, Kratt T, Preyer S, Konigsrainer A. Surgical management of an esoph-agotracheal fistula as a severe late complication of re-peated endoscopic stenting treatment. Endoscopy 2007; 39: E341–2.
19. Dogan UB, Akin MS, Yalaki S. Endoscopic closure of tracheoesophageal fistulas with the over-the- scope clip system. J Coll Physicians Surg Pak 2014;24:S193-5.
20. Silon B, Siddiqui AA, Taylor LJ, et al. Endoscopic mana-gement of esophagorespiratory fistulas: a multicenter retrospective study of techniques and outcomes. Dig Dis Sci 2017;62:424-31.
21. Dallemagne B, Weerts J, Markiewicz S, et al: Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc 2006; 20:159-165.
22. Tzifa KT, Maxwell EL, Chait P, et al: Endoscopic treatment of congenital H-type and recurrent tracheoesophageal fistula with electrocautery and histoacryl glue. Int J Pediatr Otorhinolaryngol 2006; 70:925-930.
23. Flum DR, Koepsell T, Heagerty P, et al: The nationwide frequency of major adverse outcomes in antireflux sur-gery and the role of surgeon experience, 1992-1997.J Am Coll Surg 2002; 195:611-618.
24. Cadiere GB, Himpens J, Rajan A, et al: Laparoscopic Nissen fundoplication: Laparoscopic dissection tech-nique and results. Hepatogastroenterology 1997; 44:4-10.