
 English
English
 French
French
Immunocompetant patient presenting a combination of tubercular bronchopneumonia and pulmunary embolisme
Patient immunocompétent présentant une association de bronchopneumonie tuberculeuse et d'embolie pulmonaire
Biborchi, O. Fikri, L. Amro
Department of Respiratory Medicine, Arrazi Hospital, Mohammed VI
University Hospital Center, LRMS Laboratory, Faculty of Medicine and Pharmacy, Cadi Ayyad University Marrakech, Morocco
Corresponding author:
Biborchi
Department of Respiratory Medicine, Arrazi Hospital, Mohammed VI
University Hospital Center, LRMS Laboratory, Faculty of Medicine and Pharmacy, Cadi Ayyad University
Marrakech, Morocco.
E-mail: biborchihoussam@gmail.com
ABSTRACT
Tuberculosis is a disease with thromboembolic potential; this association is very rare but can be fatal. It is reported in 1.5% to 2.5% of cases. The pathophysiological mechanism is not clear, it may be related to hypercoagulability secondary to the inflammation during the infection.
These vascular complications are particularly seen in severe and disseminated forms of pulmonary tuberculosis such as bronchopneumonia.
We report the observation of a coexistence of tuberculous bronchopneumonia and pulmonary embolism in a young patient, this explains the need to discuss preventive heparin therapy in severe forms of tuberculosis to avoid life-threatening thromboembolic complications.
KEYWORDS: tuberculosis; bronchopneumonia; thromboembolic disease; anticoagulation.
RÉSUMÉ
La tuberculose est une maladie à potentiel thromboembolique ; cette association est très rare mais peut être mortelle. Elle est rapportée dans 1,5 % à 2,5 % des cas. Le mécanisme physiopathologique n'est pas clair, il peut être lié à une hypercoagulabilité secondaire à l'inflammation lors de l'infection.
Ces complications vasculaires sont particulièrement observées dans les formes sévères et disséminées de tuberculose pulmonaire comme la bronchopneumonie.
Nous rapportons l'observation d'une coexistence d'une bronchopneumonie tuberculeuse et d'une embolie pulmonaire chez un patient jeune, ceci explique la nécessité d'évoquer l'héparinothérapie préventive dans les formes sévères de tuberculose pour éviter les complications thromboemboliques potentiellement mortelles.
MOTS CLÉS: tuberculose; bronchopneumonie; maladie thromboembolique; anticoagulant.
INTRODUCTION
The predisposing factors to thromboembolic disease are multiple and can be acquired or constitutional, classified in high, moderate and low risk factors. Tuberculosis is an independent risk factor, and the association with thromboembolic disease is rare, occurring in 1.5% to 2.5% of cases [1].
The pathophysiological mechanism of this association is not clear. Pulmonary embolism may accompany tuberculosis disease or occur during antibacillary therapy, especially in the initial phase of treatment and in severe forms of the disease. We report the observation of a pulmonary embolism confirmed on pulmonary scintigraphy complicating a tuberculous bronchopneumonia.
OBSERVATION
A 39-year-old male patient, BCG vaccinated, cigarette seller, low socioeconomic level, chronic smoker with 40 pack-year active, chronic alcoholic, presenting for 15 days with dyspnea of progressive aggravation associated with a productive cough bringing back greenish sputum and night sweats evolving in a context of alteration of the general state made of asthenia, anorexia and weight loss quantified at 10kg in 2 months.
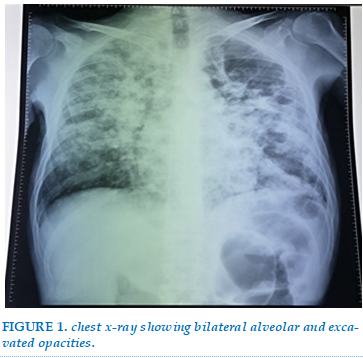
The clinical examination on admission found a conscious patient GCS 15/15th in poor general condition with a BMI of 16.35 kg/m2 , febrile at 39.8°C, mucocutaneous pallor, tachycardia, polyenic, BP 100/60 mmgh, SaO2 at 88% ambient air. The pleuropulmonary examination showed signs of respiratory struggle, and bilateral snoring on auscultation. The cardiovascular and abdominal examination were unremarkable. Chest X-ray showed diffuse confluent alveolar and bilateral excavated opacities (Figure 1).
The biological tests showed an inflammatory syndrome with a CRP of 128 mg/L, hyperleukocytosis of 15390 elements/mm3, lymphopenia of 640 elements/mm3. The D-dimer level was high.
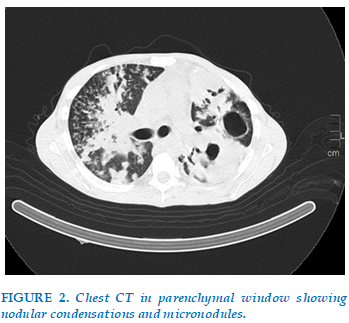
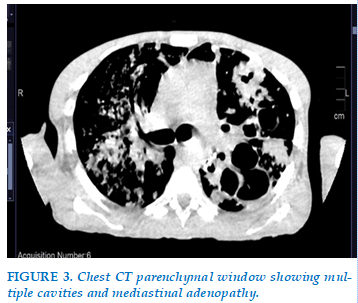
The thoracic CT scan showed diffuse nodular condensations associated with micronodules creating a budded tree aspect (Figure 2), the mediastinal window showed multiple mediastinal adenopathy. (Figure 3).
The Xpert gene in sputum and BK tests came back positive, confirming pulmonary tuberculosis. The serologies as well as the blood glucose and HBA1C were normal. The diagnosis of tuberculous bronchopneumonia was retained. The patient was put on anti-bacillary drugs. The clinical evolution marked by apyrexia; decrease of the signs of respiratory struggles, with a persistence of tachycardia.
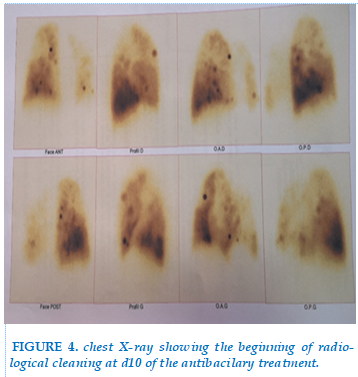
The radiological evolution showed a beginning of radiological cleaning comparing to the admission chest radiography (Figure 4).
Considering the persistence of tachycardia despite an improvement of the respiratory signs and the biological check-up, a pulmonary embolism was suspected, prompting a pulmonary perfusion scan.
The scintigraphy showed a perfusion defect in the apical segment of the left upper lobe and in the posterior segment of the upper lobe of the right lung, thus concluding to a recent pulmonary embolism (Figure 5).
The diagnosis of tuberculous bronchopneumonia complicated by pulmonary embolism was retained. The patient was put on anticoagulant treatment associated with antibacillary therapy with a good clinical evolution.
DISCUSSION
Tuberculosis is a worldwide health problem. 1/3 of the world's population is infected with Mycobacterium tuberculosis. Thromboembolic disease is a life-threatening recurrent condition, comprising two entities: pulmonary embolism and deep vein thrombosis [2].
Tuberculosis is a disease with thrombo-embolic potential, this association is rare and is found in 2.5% of cases but can be life threatening. The first cases described were in 1950 when pulmonary embolism was found in 24% of TB patients (111 patients) in a series of 634 autopsies [3]. a study in Japan of 77 patients admitted for pulmonary tuberculosis showed that 3.9% of the patients had pulmonary embolism and/or deep vein thrombosis [4].
Considering that TB is an independent risk factor for thromboembolic disease, several pathophysiological mechanisms affecting the three elements of Virchow's triad, hypercoagulability, venous stasis and endothelial dysfunction, are likely to play a role in the pathogenesis of the disease [6;11].
Disseminated tuberculosis induces the activation of mononuclear cells in the peripheral blood. the interaction with the mycobacterium is accompanied by increased synthesis of TNF alpha and Interleukin-6 [5]. These pro-inflammatory cytokines make the endothelium more thrombogenic and increasing the synthesis of coagulation proteins by the liver [7].
The presence of a hypercoagulable state during pulmonary tuberculosis results in elevated plasma fibrinogen and dysfunctional fibrinolysis, associated with decreased antithrombin III and protein C and increased platelet aggregation, resulting in endothelial damage [5;8].
The negativity of the thrombophilia test and the absence of contributing circumstances such as immobilization, surgery or the use of oestroprogestants lead to the discussion of the incrimination of tuberculosis [9].
Thromboembolic events are often concomitant with the diagnosis of TB, but sometimes they may precede the disease or occur during its treatment. Studies have shown that the risk of a thrombo-embolic event is proportional to the severity of the tuberculosis infection, which also causes hematological disorders[12].
In the series by Kouissmi et al, all patients had extensive radiological lesions. Also, Bozoky's study showed that hematological disorders are relatively common in severe pulmonary tuberculosis. Because there is a correlation between hematological disorders and the clinical severity of pulmonary tuberculosis in patients [10].
In our case the patient presents clinically a severe hypoxemic pulmonary tuberculosis, with respiratory distress. Radiological and biological: the pulmonary lesions were extended to both lung fields associated with hematological disorders: anemia; a low prothrombin level, very high inflammatory markers.
Pulmonary embolism can easily go undetected due to the nature of the symptoms common to both conditions; however, unexplained tachycardia, and an elevated D-Dimer level helped us to look for pulmonary embolism.
The use of anticoagulants in these patients is a particular situation because of the enzyme-inducing effect of rifampicin.
A higher dose of oral anticoagulation is often required to achieve an INR within the therapeutic range. Newer Xa inhibitors such as rivaroxaban or apixaban are recommended and have several advantages over traditional parenteral anticoagulant therapy such as faster onset of action, no need for a heparin introduction phase and lower hemorrhagic risk compared to standard therapy [13].
CONCLUSION
Severe pulmonary tuberculosis predisposes to the occurrence of thromboembolic events, which can be life-threatening. Pulmonary embolism may go undetected in tuberculosis infection.
It is recommended to look for thromboembolic disease in severe pulmonary tuberculosis and to consider the use of preventive anticoagulation [13;9].
CONFLICT OF INTEREST
Non.
REFERENCE
| 1. Kouissmi H, Laine M, Bourqadi JE, Iraqi G. Association deep venous thrombosis with pulmonary tuberculosis. Egyptian Journal of Chest Diseases and Tuberculosis 2013 ;62 : 541-543. |
| 2. Hamida Kwas 1, Sonia Habibech, Ines Zendah, Imen Elmjendel, Habib Ghedira Pulmonary embolism and tuberculosis asian cardiovasc thorac 2014 May;22(4):487-90. |
| 3. Morgan TJ Autopsy incidence of pulmonary embolism in tuberculosis Chest 1950 18 2 171 3 PubMed Google Scholar |
| 4. Yoshitoshi Komazaki 1, Yumi Sakakibara, Hiroyuki Sakashita, Yasunari Miyazaki, Naohiko Inase Pulmonary thromboembolism with pulmonary tuberculosis 2011 Jul;86(7):717-22. |
| 5. Ogawa T, Uchida H, Kusumoto Y, Morí Y, et al. In-crease in Tumor necrosis factor alpha and interleukin 6 secreting cells in peripheral blood mononuclear cells from subjects infected with Mycobacterium tuberculo-sis Infect. Immun 1991 ;59 :3021-25. |
| 6. Suarez Ortega S, Artiles Vizcaı´no J, Balda Aguirre I, et al. Tuberculosis as risk factor for venous thrombosis. An Med Interna 1993; 10: 398–400. |
| 7. Andus T, Bauer J, Gerok W. Effects of cytokines on the liver. Hepatology 1991 ;13 :364-375. |
| 8. Amitesh Gupta, Parul Mrigpuri, Abhishek Faye, Debdutta Bandyopadhyay, and Rupak Singla Pulmonary tuberculosis - An emerging risk factor for venous thromboembolism: A case series and review of literature Lung India. 2017 Jan-Feb; 34(1): 65–69. |
| 9. R. Bouchentouf Coexistence tuberculose pulmonaire et maladie veineuse throm-boembolique JOURNAL OF FUNCTIONAL VENTILATION AND PULMONOLOGY J Func Vent Pulm 2020; 35(11): 1-60 |
| 10. Bozóky G, Ruby E, Góhér I, Tóth J, Mohos A. Hematologic abnormalities in pulmonary tuberculosiss. Orv Hetil. 1997;138:1053–6. |
| 11. Robson S C, White N. W, Aronson I, Woolgar R, Good-man H, Jacobs P. Acute phase response and the hyper-coagulable state in pulmonary tuberculosis. Br J Hae-matol 1996; 93:423-427. |
| 12. Hye young P, Jae-Young P. Clinic al characteristics of coexisting pulmonary thromboembolism in patients with respiratory tuberculosis. The American Journal of the Medical Sciences 2017 ;353(2) :166-171 |
| 13. Cabral KP, Ansell JE. The role of factor Xa inhibitors in venous thromboembolism treatment. Vasc Health Risk Manag. 2015;11:117–23 |
Figures

REFERENCE
| 1. Kouissmi H, Laine M, Bourqadi JE, Iraqi G. Association deep venous thrombosis with pulmonary tuberculosis. Egyptian Journal of Chest Diseases and Tuberculosis 2013 ;62 : 541-543. |
| 2. Hamida Kwas 1, Sonia Habibech, Ines Zendah, Imen Elmjendel, Habib Ghedira Pulmonary embolism and tuberculosis asian cardiovasc thorac 2014 May;22(4):487-90. |
| 3. Morgan TJ Autopsy incidence of pulmonary embolism in tuberculosis Chest 1950 18 2 171 3 PubMed Google Scholar |
| 4. Yoshitoshi Komazaki 1, Yumi Sakakibara, Hiroyuki Sakashita, Yasunari Miyazaki, Naohiko Inase Pulmonary thromboembolism with pulmonary tuberculosis 2011 Jul;86(7):717-22. |
| 5. Ogawa T, Uchida H, Kusumoto Y, Morí Y, et al. In-crease in Tumor necrosis factor alpha and interleukin 6 secreting cells in peripheral blood mononuclear cells from subjects infected with Mycobacterium tuberculo-sis Infect. Immun 1991 ;59 :3021-25. |
| 6. Suarez Ortega S, Artiles Vizcaı´no J, Balda Aguirre I, et al. Tuberculosis as risk factor for venous thrombosis. An Med Interna 1993; 10: 398–400. |
| 7. Andus T, Bauer J, Gerok W. Effects of cytokines on the liver. Hepatology 1991 ;13 :364-375. |
| 8. Amitesh Gupta, Parul Mrigpuri, Abhishek Faye, Debdutta Bandyopadhyay, and Rupak Singla Pulmonary tuberculosis - An emerging risk factor for venous thromboembolism: A case series and review of literature Lung India. 2017 Jan-Feb; 34(1): 65–69. |
| 9. R. Bouchentouf Coexistence tuberculose pulmonaire et maladie veineuse throm-boembolique JOURNAL OF FUNCTIONAL VENTILATION AND PULMONOLOGY J Func Vent Pulm 2020; 35(11): 1-60 |
| 10. Bozóky G, Ruby E, Góhér I, Tóth J, Mohos A. Hematologic abnormalities in pulmonary tuberculosiss. Orv Hetil. 1997;138:1053–6. |
| 11. Robson S C, White N. W, Aronson I, Woolgar R, Good-man H, Jacobs P. Acute phase response and the hyper-coagulable state in pulmonary tuberculosis. Br J Hae-matol 1996; 93:423-427. |
| 12. Hye young P, Jae-Young P. Clinic al characteristics of coexisting pulmonary thromboembolism in patients with respiratory tuberculosis. The American Journal of the Medical Sciences 2017 ;353(2) :166-171 |
| 13. Cabral KP, Ansell JE. The role of factor Xa inhibitors in venous thromboembolism treatment. Vasc Health Risk Manag. 2015;11:117–23 |
ARTICLE INFO DOI: 10.12699/jfvpulm.14.43.2023.61
Conflict of Interest
Non
Date of manuscript receiving
25/01/2023
Date of publication after correction
25/06/2023
Article citation
Biborchi, O. Fikri, L. Amro. Immunocompetant patient presenting a combination of tubercular bronchopneumonia and pulmunary embolisme. J Func Vent Pulm 2023;43(14):61-64