
 English
English
 French
French
Study of clinical characteristics and serum procalcitonin concentration in early period neonatal infections at Ninh Thuan Province General Hospital
Étude des caractéristiques cliniques et de la concentration sérique de procalcitonine dans les infections néonatales précoces à l'hôpital général de la province de Ninh Thuan
Le Huy Thach, Le Van Thanh, Le Quoc Thang, Truong Thi Thuy Linh, Do Thuy Dung
Ninh Thuan Province General Hospital
Corresponding author: Le Huy Thach. Ninh Thuan Province General Hospital. Ninh Thuan, Vietnam.
E-mail: lh.thach67@gmail.com
ABSTRACT
Introduction. Neonatal infection early period is one of the most common causes of neonatal deaths globally.
Objective. Describe clinical and serum procalcitonin concentration in early period neonatal infections.
Subjects and Methods. Longitudinal study on 39 infants from 1 to 7 days old, treated for neonatal infections at pediatrics department, Ninh Thuan province general hospital, from January to September 2021.
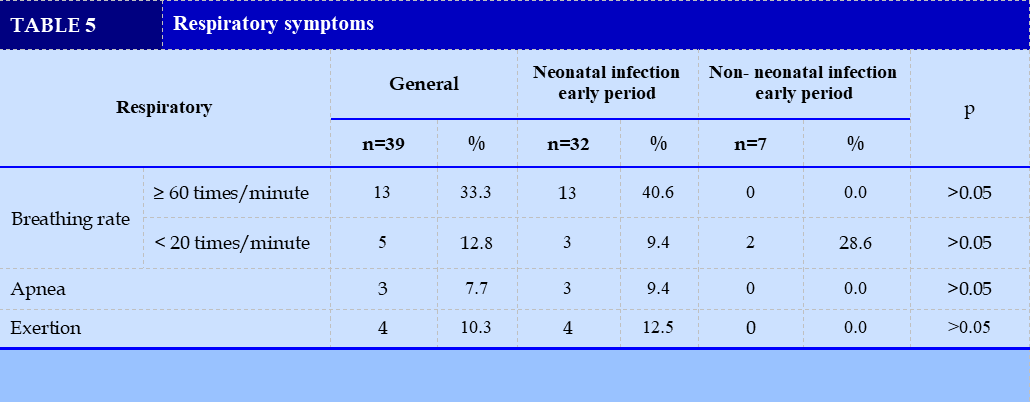
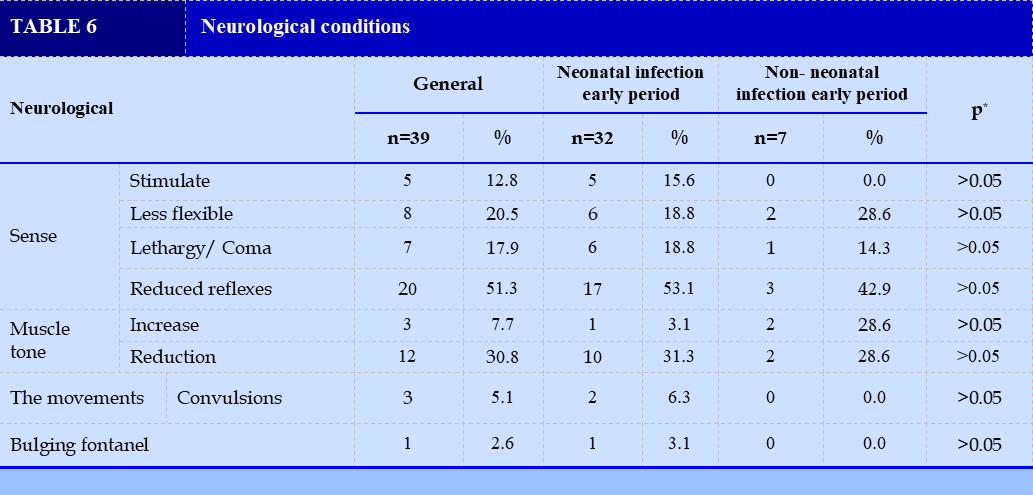
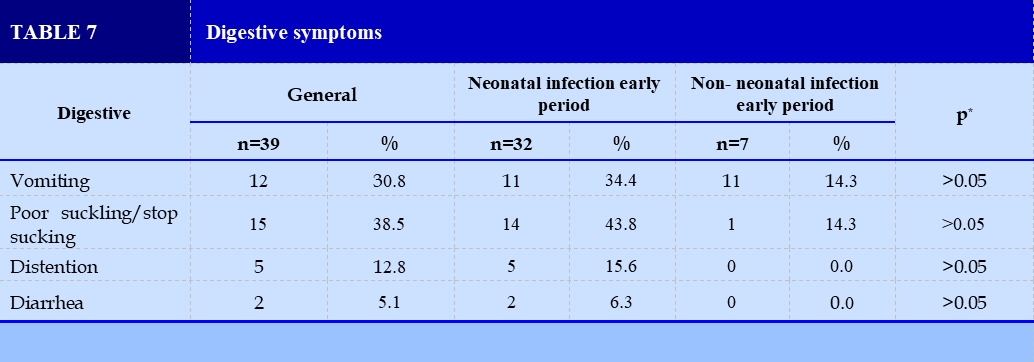
Results. Clinical. Systemic: Pale yellow skin (12.8%), fever (12.8%), cyanosis (12.8%). The cardiac: heart rate ≥160 beats/minute (15.4%), CRT >3 seconds (7.7%). Respiratory: breathing rate ≥60 beats/ minute (33.3%) and <20 beats/minute (12.8%), breathlessness (10.3%), apnoea (7.7%). Neurological: decreased reflexes (51.3%), poor muscle tone (30.8%), inflexibility (20.5%). Gastrointestinal: poor feeding/ give up sucking (38.5%), vomiting (30.8%), abdominal distention (12.8%). Median serum PCT concentration in the neonatal infection early period group (4.3 ng/ml) was higher than that in the uninfected group (p<0.05). The area under the curve was 0.96 (p<0.001) high or low PCT concentrations were able to identify neonatal infection early period with a cut-off 0.17 ng/ml with a sensitivity of 97% and a specificity of 86%.
Conclusion. The degree of clinical manifestations is highly variable and PCT is very valuable in the diagnosis of neonatal infection early period.
KEYWORDS: Neonatal infections; Procalcitonin; Ninh Thuan.
RÉSUMÉ
Introduction. L'infection néonatale au début de la période est l'une des causes les plus fréquentes de décès néonatals dans le monde.
Objectif. Décrire la concentration clinique et sérique de procalcitonine dans les infections néonatales précoces.
Sujets et méthodes. Étude longitudinale sur 39 nourrissons âgés de 1 à 7 jours, traités pour des infections néonatales au service de pédiatrie, hôpital général de la province de Ninh Thuan, de Janvier à Septembre 2021.
Résultats. Clinique. Systémique : peau jaune pâle (12,8 %), fièvre (12,8 %), cyanose (12,8 %). Le cardiaque: fréquence cardiaque ≥160 battements/minute (15,4 %), CRT > 3 secondes (7,7 %). Respiratoire: fréquence respiratoire ≥60 battements/minute (33,3 %) et <20 battements/minute (12,8 %), essoufflement (10,3 %), apnée (7,7 %). Neurologique: diminution des réflexes (51,3 %), faible tonus musculaire (30,8 %), inflexibilité (20,5 %). Gastro-intestinal: mauvaise alimentation/arrêt de la succion (38,5 %), vomissements (30,8 %), distension abdominale (12,8 %). La concentration sérique médiane de PCT dans le groupe de période précoce d'infection néonatale (4,3 ng/ml) était plus élevée que celle du groupe non infecté (p<0,05). L'aire sous la courbe était de 0,96 (p<0,001) des concentrations élevées ou basses de PCT ont permis d'identifier une infection néonatale en période précoce avec un seuil de 0,17 ng/ml avec une sensibilité de 97 % et une spécificité de 86 %.
Conclusion. Le degré des manifestations cliniques est très variable et la PCT est très précieuse dans le diagnostic de l'infection néonatale en période précoce.
MOTS CLÉS: Infections néonatales; Procalcitonine; Ninh Thuan.
INTRODUCTION
According to statistics of the World Health Organization, in 2019 globally, 2.4 million children died in the first month of life. Approximately 7,000 infants die every day. Among the causes of death, early neonatal sepsis (ENS) is consistently the leading cause [9]. Given the high mortality rate, identifying and caring for infants with infections can be one of the biggest challenges for health care providers.
Infants with ENS quickly fall into a critical condition that is difficult to control if not diagnosed in time. Therefore, careful clinical examination and appropriate laboratory tests will help to make a better diagnosis. Blood culture is a very valuable test, but the positive rate is low and results are slow. Therefore, people have studied markers such as CRP, interleukine, procalcitonin to contribute to early diagnosis of infections in general as well as ENS in particular.
Among the above markers, procalcitonin (PCT) has been evaluated to have the best diagnostic, prognostic and follow-up value. In the study of Gender et al., PCT levels in 79 patients was low without infection (<0.1 ng/ml), while it was very high (6-53 ng/ml) in patients with severe infection. For localized infections without systemic manifestations or viral infections, PCT levels are very low [6].
Recently, Ninh Thuan Provincial General Hospital is very interested in infectious diseases, especially ENS. Research by Le Huy Thach shows that the clinical features of ENS are very diverse, the tests are not clear, and at the same time, PCT has not been studied in the diagnosis of the disease [10], although this marker has been applied in the hospital. Ninh Thuan Provincial General Hospital for a long time. Stemming from that fact, with the desire to learn about PCT concentration in the diagnosis of ENS, we carried out this study to describe the clinical features, serum PCT concentration in ENS and find out the relationship between serum procalcitonin levels with clinical and blood cultures.
METHODS
Research subjects: 39 infants aged 1-7 days old, treated for neonatal infections at Thuan Provincial General Hospital from January to September 2021.
Inclusion criteria: Infants with early infant stage from 1-7 days old, consistent with the diagnostic criteria for possible infection according to ANAES [13=4]. Diagnostic criteria are based on 3 factors: risk factors, clinical and laboratory results.
Exclusion criteria: No clinical symptoms or clinical symptoms but improvement without use or change of antibiotics. There were no laboratory findings of early neonatal sepsis.
Methods
Study design: Longitudinal follow-up.
Sample size and sampling method: Convenient sample size and implementation of convenience method.
Data processing and analysis: The data were coded and analyzed by SPSS software, using Khi2 test and Fisher's exact test, with statistical significance when p<0.05.
RESULTS
Clinical features and serum procalcitonin levels
Clinical features
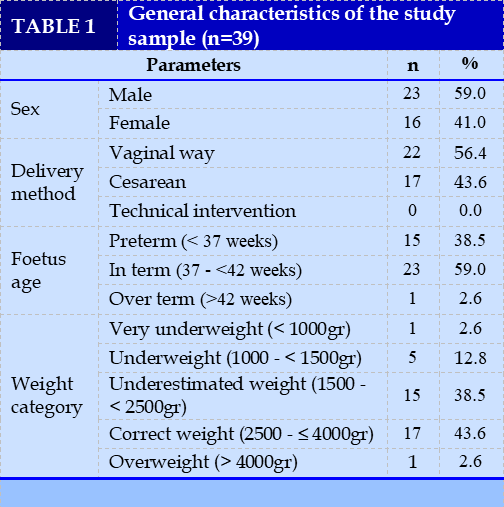
There were 23 male (59.0%) and 16 female (41.0%). (TABLE 1)
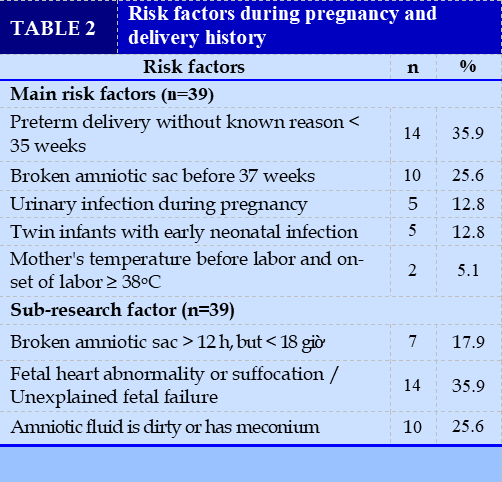
Almost of them were deliveried by a natural way (vaginal way) (58.0%). Infants with interm occuped the highest percentage (59.0%) and underweight was 38.5%. (TABLE 2)(TABLE 3)(TABLE 4)(TABLE 5)
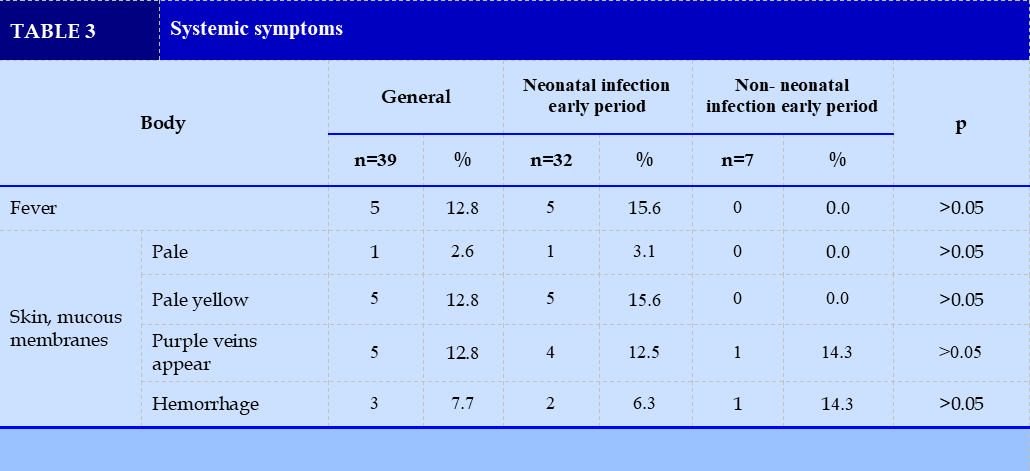
The primary study factor with the highest rate was unexplained preterm birth <35 weeks and the secondary study factor was fetal heart rate abnormality or unexplained asphyxia/fetal failure. Fever, pale yellow skin and purple veins appear are very common signs.
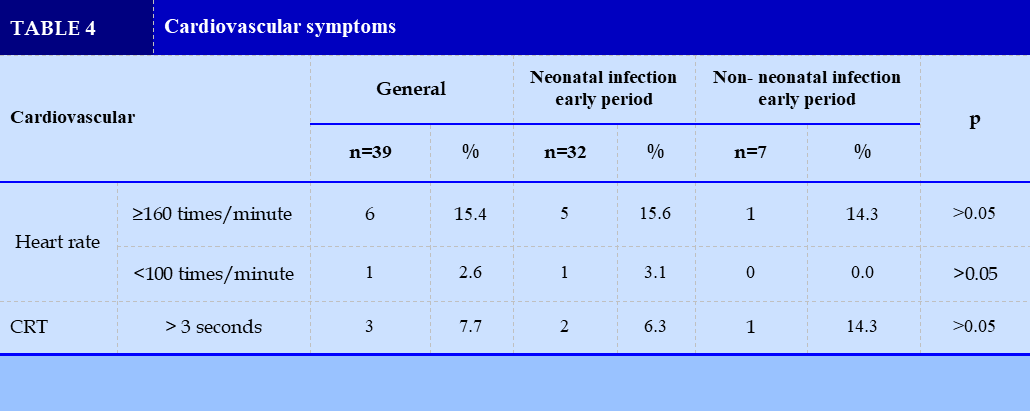
Heart rate ≥ 160 beats/min was seen in 15.4%. CRT > 3 seconds accounted for 7.7%. There was no statistically significant difference between the 2 groups in heart rate and CRT > 3 seconds (p>0.05). (TABLE 6)(TABLE 7)(TABLE 8)
The most common is tachypnea ≥ 60 times/minute (33.3%). There was no statistically significant difference between the 2 groups in respiratory expression (p>0.05). There was no statistically significant difference between the 2 groups in terms of neurological symptoms (p>0.05).
There was no statistically significant difference between the 2 groups of NTSSS and the group of no NTSSS in terms of gastrointestinal symptoms (p> 0.05).
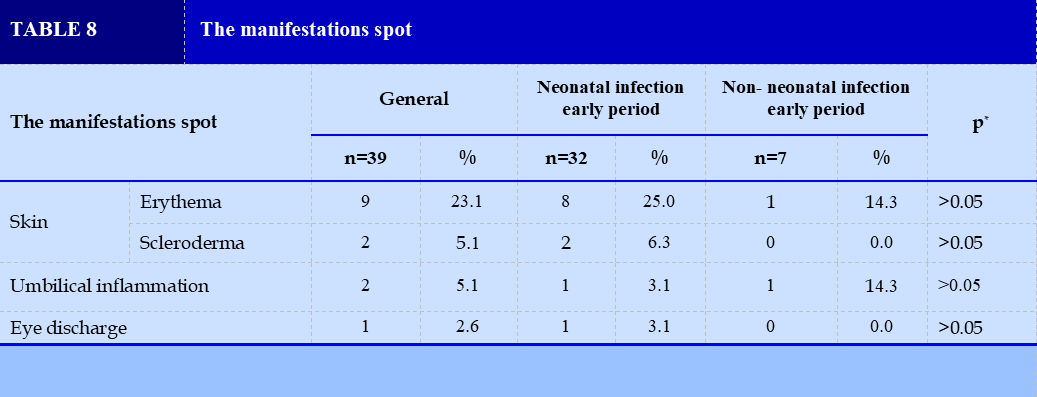
There was no statistically significant difference between the 2 groups of NTSSS and the group of no NTSSS in terms of local signs (p>0.05).
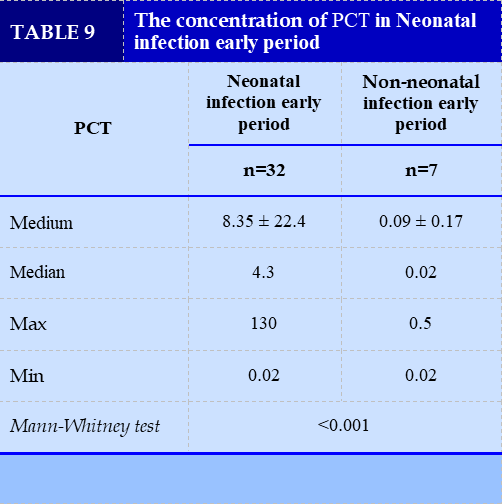
The concentration of procalcitonin levels in Neonatal infection early period (TABLE 9)
The area under the curve is 0.96 (p<0.001), and high or low PCT concentration is capable of identifying Neonatal infection early period with a cutoff point of 0.17 ng/ml with 97% sensitivity and 86% specificity.
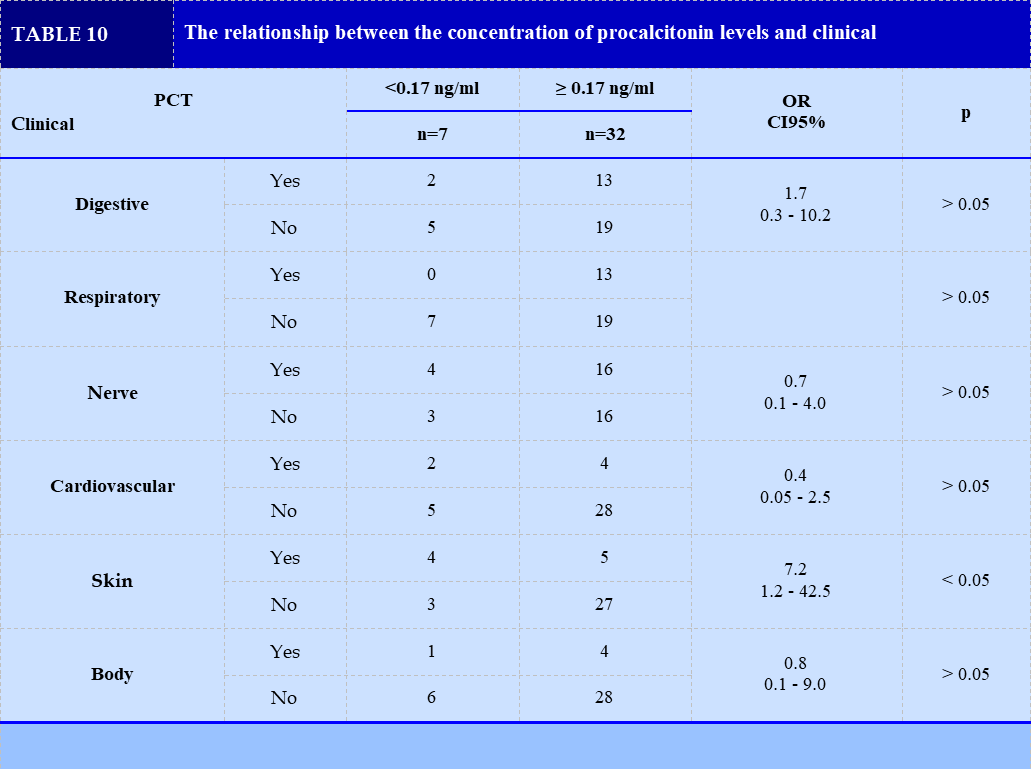
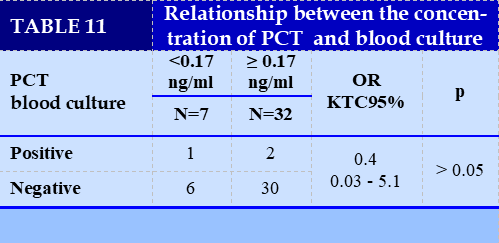
The relationship between the concentration of procalcitonin levels and clinical and blood cultures (FIGURE 1) (TABLE 10) (TABLE 11)
Only clinical manifestations in the skin had a statistically significant difference with an increase in the concentration of procalcitonin levels (p < 0.05).
There was no statistically significant difference between the increased concentration of PCT and blood culture (p>0.05).
DISCUSSION
The clinical features and Serum procalcitonin levels
The clinical features
General characteristics of the study subjects were similar to Velaphi, boys (54.6%), gestational age ≥ 37 weeks (52.7%), a cesarean delivery (53.9%) and weight ≥ 2500g (44.2). %) [11]. Regarding the study factors in the obstetric history, the results showed that unexplained preterm birth < 35 weeks and premature rupture of membranes before 37 weeks were the two most frequent primary study factors. Similar to us, Tran Quoc Viet showed that the common main research factor was spontaneous rupture of membranes < 37 weeks (25.81%), urinary tract infection during pregnancy 11.83% and mother's fever 8,60% [4]. Comparing the sub-study factors, Do Ho Tinh Tam recorded abnormal fetal heart rate or asphyxia/unexplained fetal distress at only 8.4%, lower than us, premature rupture of membranes ≥12 hours, but < 18 hours (13.7%) and amniotic fluid dirty or meconium (13.7%), similar to ours [3].
Studying 39 cases, we found that the clinical signs were different, most showed from 1 to many clinical signs and some cases had all the signs. The rate of signs appearing in the Neonatal infection early period group was higher than in the non-Neonatal infection early period group, but the difference was not statistically significant. Therefore, the clinical diagnosis of NTSSS is difficult and confusing. The NTSSS group in our study had neurological signs of decreased reflexes (53.1%), respiratory rate of ≥ 60 breaths/minute (40.6%) and poor digestion of sucking or skipping (43.8%) had the highest rate. Similar to other studies, the rate of expression in this organ is also high such as Bui Thi Hang with reduced reflexes of 35.1%, poor sucking/aborting at 31.1% [2], Le Phan Ngoc Bich frequency the number of breaths ≥ 60 breaths/minute accounted for 37.7%, poor sucking/ aborting 39.3% [1]. Do Ho Tinh Tam, rapid breathing accounted for 42%, especially this study also showed that the fever rate was 12.2% similar to ours (15.6%) [3]. Besides, our study also recorded some neurological symptoms such as convulsions (6.3%), bulging fontanels (3.1%), Mhada results in seizures of 3.0% and fontanelles swelling accounted for 10% [7].
Serum procalcitonin levels
Table 9 shows that the median serum PCT concentration of the Neonatal infection early period group was higher than that of the no-infection group (p<0.05). Similar to us, Le Phan Ngoc Bich showed that the median serum PCT concentration in the NTSSS group was 0.520 ng/ml, and the non-infection group was 0.072 ng/ml (p<0.001) [1]. Naher (2011), and Minoo Adib (2012) also showed a significant difference (p<0.05) in PCT concentrations between the two groups of Neonatal infection early period and no infection [5], [8]. This suggests that serum PCT levels are significant in differentiating Neonatal infection early period.
The value of PCT in determining Neonatal infection early period, the ROC curve (Figure 1) describes the PCT value determining Neonatal infection early period with an area under the curve equal to 0.96 (compared with the non-infectious group), with a cutoff of 0.17 ng/ml has a sensitivity of 97% and specificity of 86%. Le Phan Ngoc Bich, with PCT cut-off ≥ 0.104 ng/ml, the sensitivity is 100% and specificity is 83.9% [1].
The relationship between the concentration of procalcitonin levels and clinical and blood cultures
Besides studying the clinical and PCT concentration in Neonatal infection early period, we also wanted to find out if the PCT cut-off point of 0.17 ng/ml is related to the occurrence of clinical signs. The results of Table 10 show that only the clinical manifestations in the skin have a statistically significant difference with the increase in serum PCT concentration (p < 0.05). In other organs such as digestive, respiratory, nervous, cardiovascular, systemic, we did not find a statistically significant difference with the cut-off point of PCT ≥ 0.17 ng/ml (p>0, 05). Similarly, the study results also did not find an association between increased serum PCT concentration and blood culture (p>0.05). This may be due to our low sample size (only 39 patients) and only 3 patients with positive blood cultures.
The study of Yan et al (2017), showed that among 486 patients with sepsis who were positive for blood cultures, 254 (52.26%) were positive for Gram-negative bacteria and 202 (42.18%) were positive. against Gram-positive bacteria.
The median PCT concentration in the Gram-negative group was 2.42 ng/mL, higher than that in the Gram-positive group (0.49 ng/mL), the difference was statistically significant. with p < 0.001. The PCT cutoff value that can identify Gram-negative infections is 10.3 ng/mL, with a specificity of 80.2% [12].
CONCLUSION
Clinical symptoms in NTSSS are diverse, easy to confuse and miss, leading to delay in treatment. Symptoms are most common in the digestive, respiratory and nervous systems. PCT has very good value in diagnosing Neonatal infection early period, the area under the curve is 0.96 (p<0.001), high or low PCT concentration is able to dentify. Neonatal infection early period with cut-off point of 0.17 ng/ml, the accuracy 97% sensitivity and 86% specificity.
CONFLICT OF INTERESTS
Non.
REFERENCE
| 1. Le Phan Ngoc Bich (2018), Research on clinical characteristics and serum procalcitonin levels in early neonatal infections at Hue University of Medicine and Pharmacy Hospital, Master of Medicine Thesis, Hue University of Medicine and Pharmacy. |
| 2. Bui Thi Hang (2013), Research on the value of CRP in diagnosing early neonatal infections through the maternal-fetal route, Master's thesis of medicine by hospital resident, Hue University of Medicine and Pharmacy. |
| 3. Do Ho Tinh Tam (2016), Research on clinical characteristics, laboratory tests and treatment results of early neonatal infections in Pediatrics Department, Hue University of Medicine and Pharmacy, Master's Thesis of Medicine, University of Medicine and Pharmacy Hue. |
| 4. Tran Quoc Viet (2012), Research on some clinical characteristics and diagnostic value of peripheral blood leukocytes in early neonatal infections through maternal and fetal transmission at the Pediatrics Department, Hue University of Medicine and Pharmacy, Thesis Specialist level II, Hue University of Medicine and Pharmacy. |
| 5. Adib M., Bakhshiani Z., Navaei F., et al (2012), “Procalcitonin: a reliable marker for the diagnosis of neonatal sepsis”, Iranian journal of basic medical sciences, 15(2), 777. |
| 6. Gendrel D., Raymond J., Coste J., et al (1999), “Comparison of procalcitonin with C-reactive protein, interleukin 6 and interferon-alpha for differentiation of bacterial vs. viral infections”, The Pediatric infectious disease journal, 18(10), 875-881. |
| 7. Mhada T.V, Fredrick F, Matee M. I., et al. (2012), “Neonatal sepsis at Muhimbili National Hospital, Dar es Salaam, Tanzania; aetiology, antimicrobial sensitivity pattern and clinical outcome”, BMC public health, 12(1), 904. |
| 8. Naher B.S., et al (2011), “Role of serum procalcitonin and C-reactive protein in the diagnosis of neonatal sepsis”, Bangladesh Medical Research Council Bulletin, 37(2), 40-46. |
| 9. Simonsen K.A., et al (2014), “Early-onset neonatal sepsis”, Clinical microbiology reviews, 27(1), 21-47. |
| 10. Le Huy Thach, Phan Hung Viet, Le Van Thanh., et al (2021), “Study clinical, paraclinical features and the outcome of treatment for neonatal infections in early period at Ninh Thuan provincial general hospital”, Journal Of Functional Ventilation And Pulmonology, 37(12), 26-32. |
| 11. Velaphi S.C., Westercamp M., Moleleki M., et al. (2019), “Surveillance for incidence and etiology of early-onset neonatal sepsis in Soweto, South Africa”, PloS one, 14(4), e0214077. |
| 12. Yan S.T., Sun L. C., Jia H. B., et al (2017), “Procalcitonin levels in bloodstream infections caused by different sources and species of bacteria”, American journal of emergency medicine, 35(4), 579-583. |
| 13. Agence Nationale d’Accréditation et d’Evaluation en Santé (ANAES) (2002), “Diagnostic et traitement curatif de l’infection bactérienne précoce du nouveau-né”, Recommandations pour la pratique clinique., 4—6. |
Figures - Tables

REFERENCE
| 1. Le Phan Ngoc Bich (2018), Research on clinical characteristics and serum procalcitonin levels in early neonatal infections at Hue University of Medicine and Pharmacy Hospital, Master of Medicine Thesis, Hue University of Medicine and Pharmacy. |
| 2. Bui Thi Hang (2013), Research on the value of CRP in diagnosing early neonatal infections through the maternal-fetal route, Master's thesis of medicine by hospital resident, Hue University of Medicine and Pharmacy. |
| 3. Do Ho Tinh Tam (2016), Research on clinical characteristics, laboratory tests and treatment results of early neonatal infections in Pediatrics Department, Hue University of Medicine and Pharmacy, Master's Thesis of Medicine, University of Medicine and Pharmacy Hue. |
| 4. Tran Quoc Viet (2012), Research on some clinical characteristics and diagnostic value of peripheral blood leukocytes in early neonatal infections through maternal and fetal transmission at the Pediatrics Department, Hue University of Medicine and Pharmacy, Thesis Specialist level II, Hue University of Medicine and Pharmacy. |
| 5. Adib M., Bakhshiani Z., Navaei F., et al (2012), “Procalcitonin: a reliable marker for the diagnosis of neonatal sepsis”, Iranian journal of basic medical sciences, 15(2), 777. |
| 6. Gendrel D., Raymond J., Coste J., et al (1999), “Comparison of procalcitonin with C-reactive protein, interleukin 6 and interferon-alpha for differentiation of bacterial vs. viral infections”, The Pediatric infectious disease journal, 18(10), 875-881. |
| 7. Mhada T.V, Fredrick F, Matee M. I., et al. (2012), “Neonatal sepsis at Muhimbili National Hospital, Dar es Salaam, Tanzania; aetiology, antimicrobial sensitivity pattern and clinical outcome”, BMC public health, 12(1), 904. |
| 8. Naher B.S., et al (2011), “Role of serum procalcitonin and C-reactive protein in the diagnosis of neonatal sepsis”, Bangladesh Medical Research Council Bulletin, 37(2), 40-46. |
| 9. Simonsen K.A., et al (2014), “Early-onset neonatal sepsis”, Clinical microbiology reviews, 27(1), 21-47. |
| 10. Le Huy Thach, Phan Hung Viet, Le Van Thanh., et al (2021), “Study clinical, paraclinical features and the outcome of treatment for neonatal infections in early period at Ninh Thuan provincial general hospital”, Journal Of Functional Ventilation And Pulmonology, 37(12), 26-32. |
| 11. Velaphi S.C., Westercamp M., Moleleki M., et al. (2019), “Surveillance for incidence and etiology of early-onset neonatal sepsis in Soweto, South Africa”, PloS one, 14(4), e0214077. |
| 12. Yan S.T., Sun L. C., Jia H. B., et al (2017), “Procalcitonin levels in bloodstream infections caused by different sources and species of bacteria”, American journal of emergency medicine, 35(4), 579-583. |
| 13. Agence Nationale d’Accréditation et d’Evaluation en Santé (ANAES) (2002), “Diagnostic et traitement curatif de l’infection bactérienne précoce du nouveau-né”, Recommandations pour la pratique clinique., 4—6. |
ARTICLE INFO DOI: 10.12699/jfvpulm.13.39.2022.1
Conflict of Interest
Non
Date of manuscript receiving
18/01/2022
Date of publication after correction
18/04/2022
Article citation
Le Huy T, Le Van T, Le Quoc T, Truong Thi Thuy L, Do Thuy D. Study of clinical characteristics and serum procalcitonin concentration in early period neonatal infections at Ninh Thuan Province General Hospital. J Func Vent Pulm 2022;39(13):1-7