
 English
English
 French
French
Primary seminoma of mediastinum: case report
Primary seminoma of mediastinum: case report
Sabur¹, R. Taoufiq¹, D. Lamboni², Wafae El Aamadi¹, O. Amelal¹, I. Lefqih¹, M. Bouchikh¹,³, A. Achir¹,³
1: Department of Thoracic Surgery CHU IBN Sina, Rabat, Morocco
2: Clinique Médico-Chirurgicale du CHU sylvanus Olympio de Lomé, Togo
3: Faculty of Medicine and Pharmacy, Mohamed V University, Rabat, Morocco
Corresponding author:
Sabur. Department of Thoracic Surgery CHU IBN SINA
Rabat, Morocco
E-mail: sabur.safa03@gmail.com
ABSTRACT
Mediastinal seminomas are very rare germ cell tumor that occur in the mediastinum. The present study reports the case of a 28-year old male who was treated for a primary mediastinal seminoma revealed by chest pain associated with chest tightness.
Thoracic computed tomography (CT) scan showed a heterogeneous mass in the right anterior mediastinum. Complete excision of the tumor was possible. The surgical procedure consisted of a complete mass resection. Anatomical pathology and immunohistochemistry studies concluded to a primary mediastinal seminoma. The patient has received radio-chemotherapy after surgery. The last follow-up date was January 2021 and the patient has remained disease-free for 15 months
KEYWORDS: seminoma; mediastinum; surgery.
RÉSUMÉ
Les séminomes médiastinaux sont des tumeurs germinales très rares qui surviennent dans le médiastin. La présente étude rapporte le cas d'un homme de 28 ans qui a été traité pour un séminome médiastinal primitif révélé par des douleurs thoraciques associées à une oppression thoracique.
La tomodensitométrie (TDM) thoracique a montré une masse hétérogène dans le médiastin antérieur droit. L'exérèse complète de la tumeur était possible. Le geste chirurgical a consisté en une résection massive complète. Des études d'anatomopathologie et d'immunohistochimie ont conclu à un séminome médiastinal primitif. Le patient a reçu une radio-chimiothérapie après la chirurgie. La dernière date de suivi était janvier 2021 et le patient est resté sans maladie pendant 15 mois.
MOTS CLÉS: séminome; médiastin; chirurgie.
INTRODUCTION
Mediastinal seminomas are a very rare germ cell tumor that occur in the mediastinum, they are distinguished from other primary malignant germ cell tumors of the mediastinum by a very slow growth pattern and limited potential for metastasis. Symptoms are not very characteristic, and many patients are often asymptomatic with incidental findings. The management of these tumors has been well codified, the first-line treatment is based on chemotherapy and radiation.
Nowadays, surgical excision has limited indications in the treatment of Mediastinal seminomas.
CASE REPORT
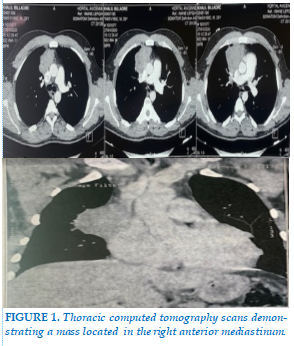
We report the case of a 28-years-old patient with no specific medical-surgical history. The patient had presented, 03 months prior to his admission, an anterior chest pain associated with chest tightness in weight loss context calculated at 05Kg. The physical examination was without particularity. Thoracic computed tomography (CT) scan showed a heterogeneous mass in the right anterior mediastinum between the trachea and the superior vena cava, with a 75 mm long axis with irregular contours without vascular compression on the right side (figure 1), the radiological aspect of which suggested a mediastinal germ cell tumor.
Tumor markers Alpha-fetoprotein(AFP), beta-human chorionic gonadotropin (β-hCG) were normal.
Lactate dehydrogenase (LDH) was elevated. The rest of blood tests were in normal ranges. Integral excision of the tumor was possible. Thus, a right anterolateral thoracotomy was performed with selective intubation on the left. Exploration found a mass in the right anterior mediastinum in close contact with neighboring vessels and an invasion of the phrenic nerve. The surgical procedure consisted of a complete mass resection with sacrifice of the right phrenic nerve. The postoperative evolution was favorable. Pathological and immunohistochemistry studies concluded a primary mediastinal seminoma classified as pT2NxMx. Excision margins were safe. No abnormalities were found in Abdominal CT scan and testicular ultrasound. The patient has received radio-chemotherapy. Regular follow-up was initiated thereafter. The last follow-up date was January 2021 and the patient has remained disease-free for 15 months.
DISCUSSION
Germ cell tumors (GCTs) are uncommon tumors of young people. They are located essentially in the gonad. Extra gonadal location is rare and is distributed along the median axis of the body. These extra gonadal germinal tumors derive from germinal cells distributed at different sites without necessarily having a testicular focus. Two different concepts have been developed for the formation of GCTs, some studies suggest that this distribution is the consequence of abnormal cell migration during embryogenesis. Another theory suggests that extra gonadal germ cell tumors develop from the malignant transformation of germ cells distributed in the liver, bone marrow and brain during embryogenesis to provide regulatory functions at these sites or to participate in important hematological or immunological genetic processes [1-2-3]. The mediastinum is the most common extra gonadal site for the development of GCTs [3]. In adults, mediastinal germ cell tumors account for 10 to 15% of all mediastinal tumors [4]. In practice, they are classified according to their histogenesis and therapeutic possibilities into seminomas, non-seminomatous and teratomas [2-4].
The primary mediastinal seminoma (PMS) is a rare tumor. It occurs almost only in young males (median age 33 years). It is most often located in the anterior mediastinum [5-6]. The clinical signs are common to the different varieties of GCTs. The most common symptoms are dyspnea, chest pain, irritating cough, fever, vena cava syndrome and fatigue [2-3]. However, it should be noted that 20 to 40% of patients are asymptomatic at the time of diagnosis [7]. The diagnosis is oriented by an X-ray of the thorax and Thoracic computed tomography. It is confirmed by histopathology analysis. Most often, the mediastinal [9].
GCTs are primitive and metastasis of a testicular tumor is exceptional but it is important to examine the testes and perform an ultrasound systematically [1-2].
Pathological diagnosis must be associated with an evaluation of serum tumor markers’ levels. A high level of one of the tumor markers, alpha-fetoprotein (AFP), beta human chorionic gonadotropin (β-hCG), and lactate dehydrogenase (LDH) may indicate the presence of a GCT [1-8]. In case of primary mediastinal seminoma, the serum level of the tumor markers β-hCG and LDH is classically normal. A moderate elevation of these tumor markers does not contradict the diagnosis [2]. AFP can help guide the diagnosis of GCTs since it is not produced by seminomas [8].
The therapeutic management of PMS has been well codified by comparison with non-seminomatous GCTs. Patients with early-stage mediastinal seminoma are curable by complete surgical resection followed by radiation therapy. All other advanced-stage patients should receive initial cisplatin-based chemotherapy (combination chemotherapy with etoposide and bleomycin) [9]. In the case of a large tumor, chemotherapy is administered initially. The surgical excision is then performed on any remaining disease if deemed resectable on imaging. Surgical intervention depends on the location of the tumor.
As the majority of mediastinal seminomas occur in the anterior mediastinum, a sternotomy, thoracotomy, VATS, or robotic surgical technique can be used in the removal of either an anterior or posterior seminoma [10]. In the individuals who are considered not to be good candidates for combination chemotherapy and who have tumors in the mediastinum, radiation therapy is an acceptable initial treatment .
When aggressive radiation and chemotherapy treatments are utilized, seminomas are curable no matter the size. The recommended initial treatment has transitioned from only radiation to cisplatin-based combination chemotherapy. The prognosis of patients who undergo surgical treatment for mediastinal seminoma is poor[10]. Almost half of the tumors recur post-op. Over the years, newer treatment regimens have increased remission rates to over 80% as well as increased the 5-year survival rate. Recent studies have shown survival rates > 90% when cisplatin-based chemotherapy is started early [2-10-11].
CONCLUSION
The primary mediastinal seminoma are a relatively rare malignant disorder. These tumors are curable by radiochemotherapy. Surgery has limited indications. Overall, the younger the patient, the better the prognosis they may have based on their ability to manage more aggressive treatment.
CONFLICT OF INTERESTS
Non.
REFERENCE
| 1. Busch J, Seidel C, Zengerling F. Male Extragonadal Germ Cell Tumors of the Adult. Oncol Res Treat. 2016;39(3):140-144. |
| 2. Chetaille B, Massard G, Falcoz PE. Les tumeurs germinales du médiastin: anatomopathologie, classification, tératomes et tumeurs malignes. Rev Pneumol Clin. 2010;66(1):63-70. |
| 3. Hanna N, Timmerman R, Foster RS, et al. Extragonadal Germ Cell Tumors. In: Kufe DW, Pollock RE, Weichselbaum RR, et al., editors. Holland-Frei Cancer Medicine. 6th edition. Hamilton (ON): BC Decker; 2003. |
| 4. Mishra S, Das Majumdar SK, Sable M, Parida DK. Primary malignant mediastinal germ cell tumors: A single institutional experience. South Asian J Cancer. 2020;9(1):27-29. |
| 5. Napieralska A, Majewski W, Osewski W, Miszczyk L. Primary mediastinal seminoma. J Thorac Dis. 2018;10(7):4335-4341 |
| 6. Xu J, Zhao J, Geng S, et al. Primary seminoma arising in the middle mediastinum: A case report. Oncol Lett. 2016;12(1):348-350. |
| 7. Takeda S, Miyoshi S, Ohta M, Minami M, Masaoka A, Matsuda H. Primary germ cell tumors in the mediastinum: a 50-year experience at a single Japanese institution. Cancer. 2003;97(2):367-376. |
| 8. Petrova D, Kraleva S, Muratovska L, Crcareva B. Primary Seminoma Localized in Mediastinum: Case Report. Open Access Maced J Med Sci. 2019;7(3):384-387. Published 2019 Jan 25. |
| 9. Hainsworth JD, Greco FA. Germ cell neoplasms and other malignancies of the mediastinum. Cancer Treat Res. 2001;105:303-325. |
| 10. Bishop MA, Kyriakopoulos C. Mediastinal Seminoma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; December 1, 2020. |
| 11. Scheckel CJ, Kosiorek HE, Butterfield R, Ho TH, Hilal T. Germ Cell Tumors with Malignant Somatic Transformation: A Mayo Clinic Experience [published correction appears in Oncol Res Treat. 2019;42(6):354]. Oncol Res Treat. 2019;42(3):95-100. |
Figure
REFERENCE
| 1. Busch J, Seidel C, Zengerling F. Male Extragonadal Germ Cell Tumors of the Adult. Oncol Res Treat. 2016;39(3):140-144. |
| 2. Chetaille B, Massard G, Falcoz PE. Les tumeurs germinales du médiastin: anatomopathologie, classification, tératomes et tumeurs malignes. Rev Pneumol Clin. 2010;66(1):63-70. |
| 3. Hanna N, Timmerman R, Foster RS, et al. Extragonadal Germ Cell Tumors. In: Kufe DW, Pollock RE, Weichselbaum RR, et al., editors. Holland-Frei Cancer Medicine. 6th edition. Hamilton (ON): BC Decker; 2003. |
| 4. Mishra S, Das Majumdar SK, Sable M, Parida DK. Primary malignant mediastinal germ cell tumors: A single institutional experience. South Asian J Cancer. 2020;9(1):27-29. |
| 5. Napieralska A, Majewski W, Osewski W, Miszczyk L. Primary mediastinal seminoma. J Thorac Dis. 2018;10(7):4335-4341 |
| 6. Xu J, Zhao J, Geng S, et al. Primary seminoma arising in the middle mediastinum: A case report. Oncol Lett. 2016;12(1):348-350. |
| 7. Takeda S, Miyoshi S, Ohta M, Minami M, Masaoka A, Matsuda H. Primary germ cell tumors in the mediastinum: a 50-year experience at a single Japanese institution. Cancer. 2003;97(2):367-376. |
| 8. Petrova D, Kraleva S, Muratovska L, Crcareva B. Primary Seminoma Localized in Mediastinum: Case Report. Open Access Maced J Med Sci. 2019;7(3):384-387. Published 2019 Jan 25. |
| 9. Hainsworth JD, Greco FA. Germ cell neoplasms and other malignancies of the mediastinum. Cancer Treat Res. 2001;105:303-325. |
| 10. Bishop MA, Kyriakopoulos C. Mediastinal Seminoma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; December 1, 2020. |
| 11. Scheckel CJ, Kosiorek HE, Butterfield R, Ho TH, Hilal T. Germ Cell Tumors with Malignant Somatic Transformation: A Mayo Clinic Experience [published correction appears in Oncol Res Treat. 2019;42(6):354]. Oncol Res Treat. 2019;42(3):95-100. |
ARTICLE INFO DOI: 10.12699/jfvpulm.13.39.2022.36
Conflict of Interest
Non
Date of manuscript receiving
18/01/2022
Date of publication after correction
18/04/2022
Article citation
Sabur, R. Taoufiq, D. Lamboni, Wafae El Aamadi, O. Amelal, I. Lefqih, M. Bouchikh, A. Achir. Primary seminoma of mediastinum. J Func Vent Pulm 2022;39(13):36-38