
 English
English
 French
French
Relationship between obstructive sleep apnea syndrome and asthma in children
Relation entre le syndrome d'apnées obstructives du sommeil et l'asthme chez les enfants
Le Nguyen- Ngoc-Quynh1,2, Mai Nguyen-Thi-Thanh2, Timothy Craig4, Sy Duong-Quy 3,4,5
1: Department of Allergy, Immunology, and Rheumatology, National Children's Hospital, Hanoi, Vietnam
2: Department of Pediatrics, Hanoi Medical University, Hanoi, Vietnam
3: Immuno-Allergology Division, Hershey Medical Center, Penn State Medical College, Hershey, PA, USA
4: Bio-Medical Research Center, Lam Dong Medical College, Dalat city, Lam Dong province, Vietnam
5: Education and Clinical Research Center, Vietnam Society of Sleep medicine, Dalat city, Lam Dong province, Vietnam
Corresponding author:
Sy DUONG-QUY. Education and Clinical Research Center, Vietnam Society of Sleep medicine, Dalat city, Lam Dong province, Vietnam.
Email: sduongquy.jfvp@gmail.com
ABSTRACT
Obstructive sleep apnea (OSA) and asthma are closely related. Both are highly prevalent chronic respiratory disorders and shared similar risk factors, interactive pathology between upper- and lower-airway, including systemic and airway inflammation, neuroimmune interactions, comorbidities such as allergic rhinitis, gastroesophageal reflux disease, obesity… Poor control of asthma and disease progression are the important factors that contribute in the development of OSA. On the other hand, undiagnosed obstructive sleep apnea affect asthma control. This article aimed to review the interaction between these two disorders in children.
OSA and asthma are common conditions. The term of "OLDOSA syndrome" may represent as a condition with important common characteristics of the two diseases. As the dual interaction between them, we should raise our awareness and provide proper therapy timely to relieve the pain of the patients. Traditional CPAP treatment can improve the asthma symptoms in those people. However, there are still some limitations. Further definitive confirmation completed by large randomized controlled trials, as well as an evaluation to analyze the lower airway structure and function in the two conditions, are still necessary.
KEYWORDS: Asthma; Obstructive sleep apnea; Overlap syndrome; Pathophysiology; Children.
RÉSUMÉ
L’apnée obstructive du sommeil (AOS) et l’asthme sont étroitement liés. Les deux sont des troubles respiratoires chroniques très répandus et partagent des facteurs de risque similaires, une pathologie interactive entre les voies respiratoires supérieures et inférieures, y compris une inflammation systémique et des voies respiratoires, des interactions neuro-immunes, des comorbidités telles que la rhinite allergique, le reflux gastro-œsophagien, l'obésité… Mauvais contrôle de l'asthme et de la maladie. la progression sont les facteurs importants qui contribuent au développement de l’AOS. D’un autre côté, l’apnée obstructive du sommeil non diagnostiquée affecte le contrôle de l’asthme. Cet article visait à passer en revue l’interaction entre ces deux troubles chez l’enfant.
L’AOS et l’asthme sont des affections courantes. Le terme « syndrome d'OLDOSA » peut représenter une affection présentant d'importantes caractéristiques communes aux deux maladies. En raison de la double interaction entre eux, nous devons accroître notre conscience et fournir une thérapie appropriée en temps opportun pour soulager la douleur des patients. Le traitement CPAP traditionnel peut améliorer les symptômes de l’asthme chez ces personnes. Cependant, il existe encore certaines limites. Une confirmation définitive supplémentaire, complétée par de grands essais contrôlés randomisés, ainsi qu'une évaluation pour analyser la structure et la fonction des voies respiratoires inférieures dans les deux conditions, sont encore nécessaires.
MOTS CLÉS: Asthme; Apnée obstructive du sommeil; Syndrome de chevauchement ; Physiopathologie; Enfants
INTRODUCTION
Asthma, also called bronchial asthma, is a chronic inflammatory disease of the airways of the lungs which symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath [1][2]. Obstructive sleep apnea is characterized by episodes of a complete (apnea) or partial collapse (hypopnea) of the upper airway with an associated decrease in oxygen saturation or arousal from sleep despite an ongoing effort to breathe [3][4]. Asthma and obstructive sleep apnea are two common respiratory diseases and tends to increase in many countries, especially in children [2][5][6].
Asthma and OSA are closely related to each other [3][7][8][9][10]. They are both chronic inflammatory conditions of the airways, sharing common risk factors such as allergic rhinitis, gastroesophageal reflux, obesity… [3][7][9][11]. Besides, these diseases are closely related to each other in terms of pathogenesis [3][9][12][13]. OSA has been found in 19 - 60% in children with mild and moderate asthma, up to 95% in children with severe asthma [3][10][14].
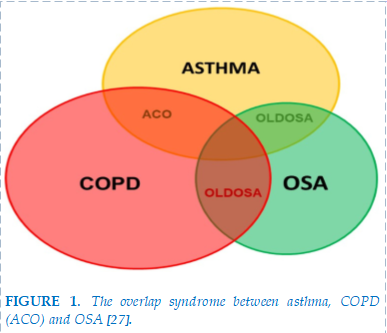
Teodorescu reported that the risk of OSA in asthma patients is 1.4 times higher than in healthy people [11]. Duong Quy Sy reported the proportion of asthmatic children with OSA is 71.2% in Vietnam [14]. Currently, OLDOSA term has been used to describe the overlap of obstructive pulmonary diseases (including bronchial asthma and chronic obstructive pulmonary disease) and obstructive sleep apnea [7][8][10][15]. Severe asthma and uncontrolled asthma increase the risk of OSA [11][16] and conversely, OSA increases the frequency of acute asthma attacks, increases severity level, and reduces the effectiveness of asthma control [12][13][14]. Kheiradish reported asthmatic children with OSA have a statistically significant higher frequency of acute asthma attacks compared to asthmatic children without OSA [13]. Therefore, GINA recommends that clinicians should screen for OSA in difficult-to-treat asthmatic patient [2][3].
This review has presented multiple acknowledged connections on epidemiology, pathophysiology, clinical manifestation, and the latest progress on diagnosis and therapies between asthma and OSA.
EPIDEMIOLOGY
Ten years ago, there were about 150 million people with asthma in the world, now there are about 300 million people, and it is predicted that by 2025 there will be 400 million people with asthma worldwide [13].
OSA and asthma are two comorbid conditions, share similar symptoms because they are related to airflow restricted and increased respiratory effort, resulting from airway narrowing during sleep [7][8][10].
In the past 20 years ago, many authors have conducted research on asthma with OSA all over the world. The prevalence of OSA in asthma patients has varied between studies’ result, between countries and gender. Cross-sectional descriptive studies showed that OSA occurs in 19- 60% of children with asthma [3][11][13][17].
In children with severe asthma and difficult-to-treat asthma, the prevalence of OSA can be up to 50- 95% [3]. Teodorescu reported that 27% of asthma patients had OSA [11]. Another multicenter study in China on 22,478 children from 5 to 12 years old showed that OSA and asthma had correlation (OR = 1.92, 95%CI: 1.34-2.76) [12]. Research by Zhihui He et al on 134 children aged 5- 18 years showed that the prevalence of asthmatic children with OSA was 57.5% [16]. In Vietnam, OSA had been diagnosed in 71,2% children with asthma [14].
In asthmatic patients, OSA acts as a mechanism contributing to worsening asthma [18] because narrowing airways in nocturnal asthma are related to sleep distribution, difficulty falling asleep, waking up early and daytime sleepiness [19]. Increased intra- abdominal pressure during OSA contributes to gastroesophageal reflux disease, bronchial hyperresponsiveness, and bronchitis [20]. Patients with poorly controlled asthma may have a high number of episodes of OSA and hypoxemia, especially during rapid eye movement sleep [18]. Teodorescu et al found that people with OSA were 3.6 times higher having uncontrolled asthma than well- controlled asthma [21].
PATHOPHYSIOLOGY
Asthma and OSA are quite common diseases in the community [1][6][22][23]. Due to the high incidence of the disease, impact of risk factors and physiological interaction between the upper and lower respiratory tracts, OSA and asthma may exist as different overlap syndromes [15] (Figure 1).
Upper airway inflammation in OSA can worsen lower airway inflammation [24]. Conversely, lower airway inflammation in asthma increases the risk of tonsil and adenoid hypertrophy, which is a risk factor that causes OSA [13][25]. This association is explained by the concept “one airway- one disease” mechanism, in which hypoxia and inflammation due to upper airway obstruction are related to the phenotype and severity of airway inflammation in lower respiratory tract [24]. Inflammatory responses to both the upper and lower respiratory tracts are related to atopy and leukotriene response. The result of this inflammation is bronchospasm, increased nasal resistance, and increased pharyngeal spasm [24][26].
Many studies have shown that asthma is an independent risk factor for OSA. Chronic inflammation in asthma affects the ability of respiratory muscles, including the upper airway dilators in children [8,9][15]. Bronchospasm in asthma causes airway collapse and increased intrathoracic pressure, thereby reducing the airway area and is associated with constriction of the pharynx and glottis during expiration [15][24].
Airway inflammation in asthma can lead to increased recruitment of neutrophils and lymphocytes into the airways, as well as recruitment of lymphocytes into the upper respiratory tract mucosa [2][8][15]. Asthma can affect the integrity and patency of the upper airway through insomnia and sleep fragmentation, consequently activating systemic inflammation and weakening the upper respiratory muscles [3][15].
Functional residual capacity during sleep in asthmatic patients is low, reducing function of the trachea on the pharynx, increasing the risk of pharyngeal collapse [15]. All mentioned factors increase the risk of OSA in these patients [3][15][16][41].
On the contrary, OSA increases the risk of asthma by increasing upper and lower respiratory resistance [9][15]. OSA causes asthma through the vagus nerve mechanism, accordingly, OSA causes upper airway collapse which will increase respiratory resistance, stimulate vagal nerve and increasing lower airway obstruction, thereby aggravating nocturnal symptoms of bronchial asthma [24].
On the other hand, intermittent nocturnal hypoxia and airway damage due to snoring may increase inflammatory response in the lower respiratory tract [24]. OSA increases abdominal pressure, causing an increased risk of gastroesophageal reflux, which is one of the risk factors for asthma [9][15].
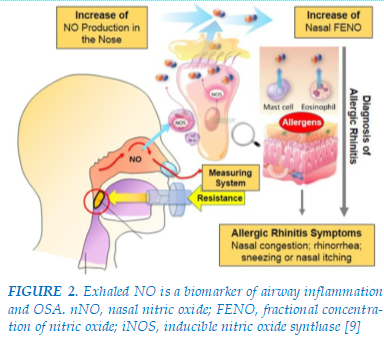
FIGURE 2. Exhaled NO is a biomarker of airway inflammation and OSA. nNO, nasal nitric oxide; FENO, fractional concentration of nitric oxide; iNOS, inducible nitric oxide synthase [9]
Direct Effects
Mechanical effects
Asthma patients with nocturnal symptoms will cause a decrease in functional residual capacity and exhaled air volume during sleep, especially during REM sleep, thereby increasing airway resistance [38]. Increased resistance leading to upper airway collapse and exacerbation of snoring and apnea [38].
Intermittent hypoxia
Repeated episodes of partial or complete upper airway obstruction during sleep due to OSA lead to intermittent hypoxia and reoxygenation [28]. The consequences lead to complex oxidative reactions, increased inflammatory responses, sympathetic tone, and endothelial dysfunction, leading to bronchial remodeling [28]. This aggravates the asthma severity.
Nerve reflex
Repeated snoring could cause damage to the soft tissue surrounding the upper airway and nasal passage due to its vibrating frequencies resulting in airway inflammation [9]. On top of the mechanical trauma, the increase in vagal tone during the apneic episodes in OSA (Muller’s maneuvers) would trigger the muscarinic receptors in the central airways and resulting in bronchoconstriction and nocturnal asthma attacks [26].
Inflammation
OSA increases local and systemic inflammatory responses, which is considered the most important factor in the effect of OSA on asthma [3][15][29]. Local inflammatory response due to mechanical mechanisms (snoring) causing mucosal damage [29]. Systemic inflammatory response characterized by an increase in pro-inflammatory cytokines and chemokines such as TNF- α, CRP, IL- 6 [9][29]. OSA patients have higher concentrations of inflammatory substances in the blood compared to healthy people
strong [29]. Excessive inflammation in the lower airways can lead to asthma, increasing the risk of acute or fatal asthma attacks [29].
Leptin
Leptin is a protein produced from adipose tissue that circulates in the blood and acts on the hypothalamus to create a feeling of satiety and increase metabolism [29,38]. Leptin levels are elevated in OSA patients [38]. Studies showed that leptin is produced locally in the airways [29] contributing to airway hyperresponsiveness and playing an important role in the pathogenesis of asthma and OSA [38].
Vascular endothelial growth factor
Vascular endothelial growth factor plays an important role in the pathogenesis of asthma and OSA [38]. VEGF is a glycoprotein sensitive to hypoxia, so OSA and asthma can promote the appearance of this factor [38][15]. Conversely, VEGF contributes to bronchitis, hyperresponsiveness, and vascular remodeling in asthmatic patients with OSA [38].
Cardiac dysfunction
Intermittent hypoxia and sleep fragmentation in OSA can increase sympathetic stimulation and increase negative intrathoracic pressure, leading to intermittent increases in left ventricular function, thereby causing, or worsening the severity of heart failure [38][15]. Heart failure leads to more difficult control of asthma [3][38][26].
Indirect effects
Glucocorticosteroids
Inhaled or oral corticosteroids are first line therapy to control asthma [2]. Yigla et al reported a high rate of OSA in patients with uncontrolled asthma treated with chronic or frequent oral corticosteroids [13][17]. The mechanism of corticosteroids affecting the airways includes inhaled corticosteroids cause fat deposition in and around the upper airway, narrowing the airway area; causes damage to airway dilator muscles, affecting airway expansion; and may worsen obesity [38][15][24].
Nasal diseases
Inflammatory infiltrates of the upper airways in asthma, increased fat deposition in the pharyngeal wall due to steroid use, or the presence of comorbidities such as obesity, cause a decrease in the horizontal diameter of the airways above [30].
Furthermore, asthmatics are often at risk of allergic and non-allergic rhinitis, nasal polyps, tonsil hypertrophy, which increases upper airway resistance, increasing negative pressure during inhalation, and risk of upper airway collapse [25][31].
Smoking
Second- hand cigarette smoke is considered a risk factor for asthma and OSA [38][15]. Cigarette smoke causes airway edema, increases airway resistance and aggravates airway spasm, causing airway collapse during sleep, resulting in aggravation of obstructive sleep apnea syndrome [38].
Obesity
Obesity is a risk factor for OSA and asthma. Obesity increases the frequency and severity of acute asthma attacks and makes it difficult to control asthma symptoms [32]. At the same time, obesity is a risk factor of OSA, a 1-unit increase in BMI increases the AHI index by 35% more (95% CI 19-53%) [30]. Another report showed a 1-unit increase in BMI will increase the risk of OSA by 1.92 times (95% CI 1.33-2.76) [30].
Gastroesophageal reflux disease
GERD occurs in 58- 62% of OSA patients [38]. Upper airway obstruction causes increased negative intrathoracic pressure, increasing the frequency of GERD, which playing an important role in the pathogenesis of asthma [9][15][26]. GERD can directly cause asthma attacks due to damage to the respiratory mucosa by vapor particles containing gastric acid and pepsin or duodenal bile acids and trypsin [38]. On the other hand, GERD indirectly causes asthma through an intermediary mechanism or reflex bronchospasm [38].
MANIFESTATIONS
There are many similar clinical manifestations between OSA and asthma, including airflow obstruction in corresponding segment, obviously sleep quality declining and daytime fatigue [3][7][8]. Both diseases often attack during the night or in the early morning. Series of cardiovascular system complications occur if poorly controlled [9][15]. Therefore, in clinical work, it is difficult to differentiate OSA from nocturnal asthma just based on patient’s complaints. Some functional assessments such as bronchial provocation/dilation test or PSG might help [4][6]. With the growing awareness of the relationship between the two diseases, some scholars defined them as "OLDOSA syndrome" to help us better stratify the therapies.
DIAGNOSIS
At present, most of the diagnostic procedures of OSA rely on PSG [4]. By monitoring overnight brain electrical activity, respiration, thoracic-abdominal motion, finger oxygen saturation, etc., physicians can get information about the distribution of sleeping state, frequency, and duration of apnea and hypoxia. By contrast, the diagnosis of asthma principally
relies on symptoms, accompanied by lung function, allergen test, etc [2]. Since OSA is often neglected in clinical work, current asthma guideline has recommended the testing for OSA in those overweight or obese patients with poorly controlled asthma. By inquiring the patient or his/her bed partner, the symptoms of snoring, witnessed apnea, excessive fatigue, or sleepiness during wakefulness, physicians can get a preliminary inspection [3][7][8].
TREATMENT
Weight loss
Weight loss is recommended for all obese children [33][34]. Obesity is a risk factor for OSA. Therefore, weight control is very important after Adenotonsillectomy surgery in the treatment of OSA. In addition to CPAP therapy, which is often recommended after AT in obese children, bariatric surgery is also an effective weight-loss treatment for children with severe apnea who are failure in losing weight or other treatments [42].
All children should receive 4 hours/week of individual physical training and play various sports (2 hours/week) and swimming (1 hour/week). Additional physical activities are also carried out according to the age groups of children, spending a lot of leisure time on outdoor games. Before and after school, children are encouraged to exercise for 10 hours/week or even more if desired [35].
Oral appliance therapy
Antibiotics
Antibiotics may reduce the size of the tonsils and adenoids in some children. This may temporarily improve OSA, but it is not necessary in all children with adenoid hypertrophy and should not be used continuously. The effect of antibiotics on OSA was evaluated in a trial of 22 children (aged 2 to 12 years) with OSA [36]. Children were randomized to receive azithromycin (12 mg/kg) or placebo on days 1 to 5, days 11 to 15, and days 21 to 25 during the 30 days of trial. There were no significant differences in two groups when assessed on PSG performed within two weeks after testing. Therefore, antibiotics are not indicated for the routine treatment of OSA in children [36].
Corticosteroid nasal spray
Upper respiratory tract inflammation is an important cause of respiratory disorders in children [3][7]. Inhaled corticosteroids reduce inflammation of upper respiratory tract mucosa, reduce size of tonsils and adenoids, and reduce severity of OSA [7][9]. On the other hand, nasal corticosteroids are effective in treating allergic rhinitis, a condition that often co-occurs with OSA in children.
Therefore, nasal corticosteroids are effective in treating mild to moderate OSA [3][7][9].
Leukotriene antagonists
Leukotrienes are a group of fatty acid chemical mediators discovered in 1979. Leukotrienes are produced in large quantities in asthma patients compared to normal people [29,39]. Recent studies show the presence of large numbers of Leukotrienes and Leukotrienes -receptors in the adenoids and tonsils in children with OSA [3][23]. This is the basis concept for using leukotriene antagonists in the treatment of mild OSA in children [3][14][25].
The study which has been done in 63 Vietnamese children with mild OSA treated with 12 weeks of montelukast, showed that nearly 50% of patients had reduced OSA symptoms and AHI index after being treated with leukotriene antagonists [25].
Surgery
Adenotonsillectomy
Adenotonsillectomy is considered as first method in treating OSA in children, especially in OSA accompanied by tonsil and adenoid hypertrophy, helping to improve parameters on PSG even though OSA symptoms may remain after surgery [6][13][25,41,42]. AT is indicated if the patient has severe OSA with AHI ≥10 event/hour [25]. Studies show the success of OSA treatment by AT are very different, ranging from 24- 100% [6][23]. A study conducted AT to treat OSA on 51 Vietnamese children and found that there was an improvement in both clinical symptoms and AHI index on polysomnography post AT [25].
Positive Airway Pressure Therapy
Positive airway pressure has been indicated in the treatment of OSA since the 1980s. CPAP therapy is frequently used to treat children who manifest moderate to severe OSA. The machine uses positive pressure to maintain airway collapse, thereby eliminating or reducing intermittent hypoxia and hypoxia. sleep fragmentation in OSA patients [6][16][37].
CONCLUSION
In summary, OSA and asthma are common conditions. The term of "OLDOSA syndrome" may represent as a condition with important common characteristics of the two diseases. As the dual interaction between them, we should raise our awareness and provide proper therapy timely to relieve the pain of the patients. Traditional CPAP treatment can improve the asthma symptoms in those people. However, there are still some limitations. Further definitive confirmation completed by large randomized controlled trials, as well as an evaluation to analyze the lower airway structure and function in the two conditions, are still necessary.
AUTHOR CONTRIBUTIONS
Conceptualization, LN-N-Q, MN-T-T, and SD-Q; methodology, LN-N-Q and SD-Q; writing—original draft preparation, LN-N-Q and SD-Q; writing—review and editing, H LN-N-Q, MN-T-T, and SD-Q; visualization, LN-N-Q, MN-T-T, and SD-Q; supervision, SD-Q; project administration, SD-Q. All authors have read and agreed to the published version of the manuscript.
FUNDING
This research received no external funding.
DATA AVAILABILITY STATEMENT
Not applicable.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
REFERENCE
| 1. Asher MI, Rutter CE, Bissell K, et al. Worldwide trends in the burden of asthma symptoms in school-aged children: Global Asthma Network Phase I cross-sectional study. Lancet Lond Engl. 2021;398(10311):1569-1580. doi:10.1016/S0140-6736(21)01450-1. |
| 2. 2020 Global Initiative for Asthma - GINA. Pocket Guideline for Asthma Management and Prevention (for Adults and Children Older 5 Years). https://ginasthma.org/wpcontent/uploads/2020/04/Main-pocket-guide_2020_04—final-wms.pdf. |
| 3. Damianaki A, Vagiakis E, Sigala I, et al. Τhe Co-Existence of Obstructive Sleep Apnea and Bronchial Asthma: Revelation of a New Asthma Phenotype? J Clin Med. 2019; 8(9): 1476. doi:10.3390/jcm8091476. |
| 4. Thorpy M. International Classification of Sleep Disorders. In: Chokroverty S, ed. Sleep Disorders Medicine: Basic Science, Technical Considerations and Clinical Aspects. Springer; 2017:475-484. doi:10.1007/978-1-4939-6578-6_27. |
| 5. Gipson K, Lu M, Kinane TB. Sleep-Disordered Breathing in Children. Pediatr Rev. 2019;40(1):3-13. doi:10.1542/pir.2018-0142. |
| 6. Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714-755. doi:10.1542/peds.2012-1672. |
| 7. Wang R, Mihaicuta S, Tiotiu A, et al. Asthma and obstructive sleep apnoea in adults and children - an up-to-date review. Sleep Med Rev. 2022;61:101564. doi:10.1016/j.smrv.2021.101564. |
| 8. Prasad B, Nyenhuis SM, Imayama I, et al. Asthma and Obstructive Sleep Apnea Overlap: What Has the Evidence Taught Us? Am J Respir Crit Care Med. 2020;201(11):1345-1357.doi:10.1164/rccm.201810-1838TR. |
| 9. Duong-Quy S. Clinical Utility Of The Exhaled Nitric Oxide (NO) Measurement With Portable Devices In The Management Of Allergic Airway Inflammation And Asthma. J Asthma Allergy. 2019 Oct 7; 12: 331-341. |
| 10. Ioachimescu OC, Janocko NJ, Ciavatta MM, et al. Obstructive Lung Disease and Obstructive Sleep Apnea (OLDOSA) cohort study: 10-year assessment. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2020;16(2):267-277. doi:10.5664/jcsm.8180. |
| 11. Teodorescu M, Barnet JH, Hagen EW, et al. Association between asthma and risk of developing obstructive sleep apnea. JAMA. 2015;313(2):156-164. doi:10.1001/jama.2014.17822. |
| 12. Li L, Xu Z, Jin X, et al. Sleep-disordered breathing and asthma: evidence from a large multicentric epidemiological study in China. Respir Res. 2015;16(1):56. doi:10.1186/s12931-015-0215-5. |
| 13. Kheirandish-Gozal L, Dayyat EA, Eid NS, et al. Obstructive sleep apnea in poorly controlled asthmatic children: effect of adenotonsillectomy. Pediatr Pulmonol. 2011; 46(9): 913-918. doi:10.1002/ ppul. 21451. |
| 14. Duong-Quy S, Nguyen-Hoang Y, Nguyen-Ngoc-Quynh L, et al. Clinical and functional characteristics of OSA in children with comorbid asthma treated by leukotriene receptor antagonist: A descriptive study. Front Neurol. 2023 Jan 4;13:1065038. doi: 10.3389/fneur.2022.1065038. PMID: 36686503; PMCID: PMC9846608. |
| 15. Ioachimescu OC, Teodorescu M. Integrating the overlap of obstructive lung disease and obstructive sleep apnoea: OLDOSA syndrome. Respirol Carlton Vic. 2013;18(3):421-431. doi:10.1111/resp.12062. |
| 16. He Z, Armoni Domany K, Nava-Guerra L, et al. Phenotype of ventilatory control in children with moderate to severe persistent asthma and obstructive sleep apnea. Sleep. 2019; 42(9): zsz130. doi:10.1093/sleep/zsz130. |
| 17. Yigla M, Tov N, Solomonov A, et al. Difficult‐to‐Control Asthma and Obstructive Sleep Apnea. J Asthma. 2003; 40 (8): 865- 871. doi:10.1081/JAS-120023577. |
| 18. Gutierrez MJ, Zhu J, Rodriguez-Martinez CE, Nino CL, Nino G. Nocturnal phenotypical features of obstructive sleep apnea (OSA) in asthmatic children. Pediatr Pulmonol. 2013 Jun;48(6):592-600. doi: 10.1002/ppul.22713. Epub 2012 Nov 30. PMID: 23203921. |
| 19. Shigemitsu H, Afshar K. Nocturnal asthma. Curr Opin Pulm Med. 2007 Jan;13(1):49-55. doi: 10.1097/MCP.0b013e328010a890. |
| 20. Lewis DA. Sleep in patients with asthma and chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2001 Mar;7(2):105-12. doi: 10.1097/00063198-200103000-00008. PMID: 11224731. |
| 21. Teodorescu M, Polomis DA, Hall SV, Teodorescu MC, Gangnon RE, Peterson AG, Xie A, Sorkness CA, Jarjour NN. Association of obstructive sleep apnea risk with asthma control in adults. Chest. 2010 Sep;138(3):543-50. doi: 10.1378/chest.09-3066. Epub 2010 May 21. PMID: 20495105; PMCID: PMC2940069. |
| 22. Mallol J, Crane J, von Mutius E, et al. The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three: A global synthesis. Allergol Immunopathol (Madr). 2013; 41 (2): 73- 85. doi:10.1016/j.aller.2012.03.001. |
| 23. Tan HL, Gozal D, Kheirandish- Gozal L. Obstructive sleep apnea in children: a critical update. Nat Sci Sleep. 2013; 5:109- 123. doi:10.2147/NSS.S51907. |
| 24. Garza N, Witmans M, Salud M, et al. The Association between Asthma and OSA in Children. Child Basel Switz. 2022;9(10):1430. doi:10.3390/children9101430. |
| 25. Tran-Minh D, Phi-Thi-Quynh A, Nguyen-Dinh P, Duong-Quy S. Efficacy of obstructive sleep apnea treatment by antileukotriene receptor and surgery therapy in children with adenotonsillar hypertrophy: A descriptive and cohort study. Front Neurol. 2022 Sep 27;13:1008310. doi: 10.3389/fneur.2022.1008310. PMID: 36237622; PMCID: PMC9552176. |
| 26. Pepito DL, Mohammed JM, Hardin KA. Obstructive Sleep Apnea and Asthma: More Than Chance? Curr Pulmonol Rep. 2021;10(2):84-91. doi:10.1007/s13665-021-00271-5. |
| 27. Duong-Quy S, Nguyen-Huu H, Hoang-Chau-Bao D, Tran-Duc S, Nguyen-Thi-Hong L, Nguyen-Duy T, Tang-Thi-Thao T, Phan C, Bui-Diem K, Vu-Tran-Thien Q, Nguyen-Ngoc-Phuong T, Nguyen-Nhu V, Le-Thi-Minh H, Craig T. Personalized Medicine and Obstructive Sleep Apnea. J Pers Med. 2022 Dec 8;12(12):2034. doi: 10.3390/jpm12122034. PMID: 36556255; PMCID: PMC9781564. |
| 28. DelRosso LM, Panek D, Redding G, et al. Obstructive Apnea and Hypopnea Length in Normal Children and Adolescents. Brain Sci. 2021;11(10):1343. doi:10.3390/brainsci11101343. |
| 29. Barnes PJ. The cytokine network in asthma and chronic obstructive pulmonary disease. J Clin Invest. 2008;118(11):3546-3556. doi:10.1172/JCI36130. |
| 30. Andersen IG, Holm JC, Homøe P. Obstructive sleep apnea in children and adolescents with and without obesity. Eur Arch Otorhinolaryngol. 2019;276(3):871-878. doi:10.1007/s00405-019-05290-2. |
| 31. Guo Y, Zhang X, Liu F, et al. Relationship between Poorly Controlled Asthma and Sleep-Related Breathing Disorders in Children with Asthma: A Two-Center Study. Can Respir J. 2021; 2021: 8850382. doi:10.1155/2021/8850382. |
| 32. Di Genova L, Penta L, Biscarini A, et al. Children with Obesity and Asthma: Which Are the Best Options for Their Management? Nutrients. 2018;10(11):1634. doi:10.3390/nu10111634. |
| 33. Capdevila OS, Kheirandish-Gozal L, Dayyat E, Gozal D. Pediatric obstructive sleep apnea: complications, management, and long-term outcomes. Proc Am Thorac Soc. 2008 Feb 15;5(2):274-82. doi: 10.1513/pats.200708-138MG. PMID: 18250221; PMCID: PMC2645258. |
| 34. Rubinstein, B.J., Baldassari, C.M. An Update on the Management of Pediatric Obstructive Sleep Apnea. Curr Treat Options Peds 2015, 1, 211–223. https://doi.org/10.1007/s40746-015-0022-8. |
| 35. Garde AJB, Gibson NA, Samuels MP, et al. Recent advances in paediatric sleep disordered breathing. Breathe Sheff Engl. 2022;18(3):220151. doi:10.1183/20734735.0151-2022. |
| 36. Don DM, Goldstein NA, Crockett DM, Ward SD. Antimicrobial therapy for children with adenotonsillar hypertrophy and obstructive sleep apnea: a prospective randomized trial comparing azithromycin vs placebo. Otolaryngol Head Neck Surg. 2005 Oct;133(4):562-8. doi: 10.1016/j.otohns.2005.05.012. PMID: 16213930. |
| 37. Chang SJ, Chae KY. Obstructive sleep apnea syndrome in children: Epidemiology, pathophysiology, diagnosis and sequelae. Korean J Pediatr. 2010;53(10):863-871. doi:10.3345/kjp.2010.53.10.863. |
| 38. Puthalapattu S, Ioachimescu OC. Asthma and obstructive sleep apnea: clinical and pathogenic interactions. J Investig Med Off Publ Am Fed Clin Res. 2014;62(4):665-675. |
| 39. Vo-Thi-Kim, A., Van-Quang, T., Nguyen-Thanh, B., Dao-Van, D., & Duong-Quy, S. The effect of medical treatment on nasal exhaled nitric oxide (NO) in patients with persistent allergic rhinitis: A randomized control study. Advances in medical sciences,2020;65(1), 182-188. |
| 40. Duong-Quy, Sy, et al. "Clinical and functional characteristics of subjects with asthma, COPD, and asthma-COPD overlap: A multicentre study in Vietnam." Canadian Respiratory Journal 2018 (2018). |
| 41. Dinh-Thi-Dieu H, Vo-Thi-Kim A, Tran-Van H, Duong-Quy S. Efficacy and adherence of auto-CPAP therapy in patients with obstructive sleep apnea: a prospective study. Multidiscip Respir Med. 2020 Jan 28;15(1):468. |
| 42. Duong-Quy S. Obstructive Sleep Apnea (OSA) in children: Fact and Challenge. J Func Vent Pulm. 2018;9(27):1-2. |
FIGURE
REFERENCE
| 1. Asher MI, Rutter CE, Bissell K, et al. Worldwide trends in the burden of asthma symptoms in school-aged children: Global Asthma Network Phase I cross-sectional study. Lancet Lond Engl. 2021;398(10311):1569-1580. doi:10.1016/S0140-6736(21)01450-1. |
| 2. 2020 Global Initiative for Asthma - GINA. Pocket Guideline for Asthma Management and Prevention (for Adults and Children Older 5 Years). https://ginasthma.org/wpcontent/uploads/2020/04/Main-pocket-guide_2020_04—final-wms.pdf. |
| 3. Damianaki A, Vagiakis E, Sigala I, et al. Τhe Co-Existence of Obstructive Sleep Apnea and Bronchial Asthma: Revelation of a New Asthma Phenotype? J Clin Med. 2019; 8(9): 1476. doi:10.3390/jcm8091476. |
| 4. Thorpy M. International Classification of Sleep Disorders. In: Chokroverty S, ed. Sleep Disorders Medicine: Basic Science, Technical Considerations and Clinical Aspects. Springer; 2017:475-484. doi:10.1007/978-1-4939-6578-6_27. |
| 5. Gipson K, Lu M, Kinane TB. Sleep-Disordered Breathing in Children. Pediatr Rev. 2019;40(1):3-13. doi:10.1542/pir.2018-0142. |
| 6. Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714-755. doi:10.1542/peds.2012-1672. |
| 7. Wang R, Mihaicuta S, Tiotiu A, et al. Asthma and obstructive sleep apnoea in adults and children - an up-to-date review. Sleep Med Rev. 2022;61:101564. doi:10.1016/j.smrv.2021.101564. |
| 8. Prasad B, Nyenhuis SM, Imayama I, et al. Asthma and Obstructive Sleep Apnea Overlap: What Has the Evidence Taught Us? Am J Respir Crit Care Med. 2020;201(11):1345-1357.doi:10.1164/rccm.201810-1838TR. |
| 9. Duong-Quy S. Clinical Utility Of The Exhaled Nitric Oxide (NO) Measurement With Portable Devices In The Management Of Allergic Airway Inflammation And Asthma. J Asthma Allergy. 2019 Oct 7; 12: 331-341. |
| 10. Ioachimescu OC, Janocko NJ, Ciavatta MM, et al. Obstructive Lung Disease and Obstructive Sleep Apnea (OLDOSA) cohort study: 10-year assessment. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2020;16(2):267-277. doi:10.5664/jcsm.8180. |
| 11. Teodorescu M, Barnet JH, Hagen EW, et al. Association between asthma and risk of developing obstructive sleep apnea. JAMA. 2015;313(2):156-164. doi:10.1001/jama.2014.17822. |
| 12. Li L, Xu Z, Jin X, et al. Sleep-disordered breathing and asthma: evidence from a large multicentric epidemiological study in China. Respir Res. 2015;16(1):56. doi:10.1186/s12931-015-0215-5. |
| 13. Kheirandish-Gozal L, Dayyat EA, Eid NS, et al. Obstructive sleep apnea in poorly controlled asthmatic children: effect of adenotonsillectomy. Pediatr Pulmonol. 2011; 46(9): 913-918. doi:10.1002/ ppul. 21451. |
| 14. Duong-Quy S, Nguyen-Hoang Y, Nguyen-Ngoc-Quynh L, et al. Clinical and functional characteristics of OSA in children with comorbid asthma treated by leukotriene receptor antagonist: A descriptive study. Front Neurol. 2023 Jan 4;13:1065038. doi: 10.3389/fneur.2022.1065038. PMID: 36686503; PMCID: PMC9846608. |
| 15. Ioachimescu OC, Teodorescu M. Integrating the overlap of obstructive lung disease and obstructive sleep apnoea: OLDOSA syndrome. Respirol Carlton Vic. 2013;18(3):421-431. doi:10.1111/resp.12062. |
| 16. He Z, Armoni Domany K, Nava-Guerra L, et al. Phenotype of ventilatory control in children with moderate to severe persistent asthma and obstructive sleep apnea. Sleep. 2019; 42(9): zsz130. doi:10.1093/sleep/zsz130. |
| 17. Yigla M, Tov N, Solomonov A, et al. Difficult‐to‐Control Asthma and Obstructive Sleep Apnea. J Asthma. 2003; 40 (8): 865- 871. doi:10.1081/JAS-120023577. |
| 18. Gutierrez MJ, Zhu J, Rodriguez-Martinez CE, Nino CL, Nino G. Nocturnal phenotypical features of obstructive sleep apnea (OSA) in asthmatic children. Pediatr Pulmonol. 2013 Jun;48(6):592-600. doi: 10.1002/ppul.22713. Epub 2012 Nov 30. PMID: 23203921. |
| 19. Shigemitsu H, Afshar K. Nocturnal asthma. Curr Opin Pulm Med. 2007 Jan;13(1):49-55. doi: 10.1097/MCP.0b013e328010a890. |
| 20. Lewis DA. Sleep in patients with asthma and chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2001 Mar;7(2):105-12. doi: 10.1097/00063198-200103000-00008. PMID: 11224731. |
| 21. Teodorescu M, Polomis DA, Hall SV, Teodorescu MC, Gangnon RE, Peterson AG, Xie A, Sorkness CA, Jarjour NN. Association of obstructive sleep apnea risk with asthma control in adults. Chest. 2010 Sep;138(3):543-50. doi: 10.1378/chest.09-3066. Epub 2010 May 21. PMID: 20495105; PMCID: PMC2940069. |
| 22. Mallol J, Crane J, von Mutius E, et al. The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three: A global synthesis. Allergol Immunopathol (Madr). 2013; 41 (2): 73- 85. doi:10.1016/j.aller.2012.03.001. |
| 23. Tan HL, Gozal D, Kheirandish- Gozal L. Obstructive sleep apnea in children: a critical update. Nat Sci Sleep. 2013; 5:109- 123. doi:10.2147/NSS.S51907. |
| 24. Garza N, Witmans M, Salud M, et al. The Association between Asthma and OSA in Children. Child Basel Switz. 2022;9(10):1430. doi:10.3390/children9101430. |
| 25. Tran-Minh D, Phi-Thi-Quynh A, Nguyen-Dinh P, Duong-Quy S. Efficacy of obstructive sleep apnea treatment by antileukotriene receptor and surgery therapy in children with adenotonsillar hypertrophy: A descriptive and cohort study. Front Neurol. 2022 Sep 27;13:1008310. doi: 10.3389/fneur.2022.1008310. PMID: 36237622; PMCID: PMC9552176. |
| 26. Pepito DL, Mohammed JM, Hardin KA. Obstructive Sleep Apnea and Asthma: More Than Chance? Curr Pulmonol Rep. 2021;10(2):84-91. doi:10.1007/s13665-021-00271-5. |
| 27. Duong-Quy S, Nguyen-Huu H, Hoang-Chau-Bao D, Tran-Duc S, Nguyen-Thi-Hong L, Nguyen-Duy T, Tang-Thi-Thao T, Phan C, Bui-Diem K, Vu-Tran-Thien Q, Nguyen-Ngoc-Phuong T, Nguyen-Nhu V, Le-Thi-Minh H, Craig T. Personalized Medicine and Obstructive Sleep Apnea. J Pers Med. 2022 Dec 8;12(12):2034. doi: 10.3390/jpm12122034. PMID: 36556255; PMCID: PMC9781564. |
| 28. DelRosso LM, Panek D, Redding G, et al. Obstructive Apnea and Hypopnea Length in Normal Children and Adolescents. Brain Sci. 2021;11(10):1343. doi:10.3390/brainsci11101343. |
| 29. Barnes PJ. The cytokine network in asthma and chronic obstructive pulmonary disease. J Clin Invest. 2008;118(11):3546-3556. doi:10.1172/JCI36130. |
| 30. Andersen IG, Holm JC, Homøe P. Obstructive sleep apnea in children and adolescents with and without obesity. Eur Arch Otorhinolaryngol. 2019;276(3):871-878. doi:10.1007/s00405-019-05290-2. |
| 31. Guo Y, Zhang X, Liu F, et al. Relationship between Poorly Controlled Asthma and Sleep-Related Breathing Disorders in Children with Asthma: A Two-Center Study. Can Respir J. 2021; 2021: 8850382. doi:10.1155/2021/8850382. |
| 32. Di Genova L, Penta L, Biscarini A, et al. Children with Obesity and Asthma: Which Are the Best Options for Their Management? Nutrients. 2018;10(11):1634. doi:10.3390/nu10111634. |
| 33. Capdevila OS, Kheirandish-Gozal L, Dayyat E, Gozal D. Pediatric obstructive sleep apnea: complications, management, and long-term outcomes. Proc Am Thorac Soc. 2008 Feb 15;5(2):274-82. doi: 10.1513/pats.200708-138MG. PMID: 18250221; PMCID: PMC2645258. |
| 34. Rubinstein, B.J., Baldassari, C.M. An Update on the Management of Pediatric Obstructive Sleep Apnea. Curr Treat Options Peds 2015, 1, 211–223. https://doi.org/10.1007/s40746-015-0022-8. |
| 35. Garde AJB, Gibson NA, Samuels MP, et al. Recent advances in paediatric sleep disordered breathing. Breathe Sheff Engl. 2022;18(3):220151. doi:10.1183/20734735.0151-2022. |
| 36. Don DM, Goldstein NA, Crockett DM, Ward SD. Antimicrobial therapy for children with adenotonsillar hypertrophy and obstructive sleep apnea: a prospective randomized trial comparing azithromycin vs placebo. Otolaryngol Head Neck Surg. 2005 Oct;133(4):562-8. doi: 10.1016/j.otohns.2005.05.012. PMID: 16213930. |
| 37. Chang SJ, Chae KY. Obstructive sleep apnea syndrome in children: Epidemiology, pathophysiology, diagnosis and sequelae. Korean J Pediatr. 2010;53(10):863-871. doi:10.3345/kjp.2010.53.10.863. |
| 38. Puthalapattu S, Ioachimescu OC. Asthma and obstructive sleep apnea: clinical and pathogenic interactions. J Investig Med Off Publ Am Fed Clin Res. 2014;62(4):665-675. |
| 39. Vo-Thi-Kim, A., Van-Quang, T., Nguyen-Thanh, B., Dao-Van, D., & Duong-Quy, S. The effect of medical treatment on nasal exhaled nitric oxide (NO) in patients with persistent allergic rhinitis: A randomized control study. Advances in medical sciences,2020;65(1), 182-188. |
| 40. Duong-Quy, Sy, et al. "Clinical and functional characteristics of subjects with asthma, COPD, and asthma-COPD overlap: A multicentre study in Vietnam." Canadian Respiratory Journal 2018 (2018). |
| 41. Dinh-Thi-Dieu H, Vo-Thi-Kim A, Tran-Van H, Duong-Quy S. Efficacy and adherence of auto-CPAP therapy in patients with obstructive sleep apnea: a prospective study. Multidiscip Respir Med. 2020 Jan 28;15(1):468. |
| 42. Duong-Quy S. Obstructive Sleep Apnea (OSA) in children: Fact and Challenge. J Func Vent Pulm. 2018;9(27):1-2. |
ARTICLE INFO DOI: 10.12699/jfvpulm.15.45.2024.07
Conflict of Interest
Non
Date of manuscript receiving
11/9/2023
Date of publication after correction
25/01/2024
Article citation
Le Nguyen- Ngoc-Quynh, Mai Nguyen-Thi-Thanh, Timothy Craig, Sy Duong-Quy. Relationship between obstructive sleep apnea syndrome and asthma in children. J Func Vent Pulm 2024;45(15):7-13