
 English
English
 French
French
Diagnosis and management of obstructive sleep apnea in patients with chronic obstructive pulmonary disease
Diagnostic et prise en charge de l'apnée obstructive du sommeil chez les patients atteints de la broncho-pulmonaire chronique obstructive
Duc Nguyen-Hong1*, Nhi Nguyen-Thi-Y2*, Quy Duong-Minh2, Nghia Dam-Trung2, Bang Le-Van2, Sy Duong-Quy3,4
*: Co-first authors
1: Respiratory Department. Phoi Viet Clinic. Ho Chi Minh city, Vietnam
2: Sleep Lab Unit. University of Medicine and Pharmacy - Hue University. Hue city, Vietnam
3: Sleep Lab Center. Lam Dong Medical College. Dalat city, Vietnam
4: Immuno-Allergology Division. Hershey Medical Center. Penn State Medical College. PA, USA
Corresponding author: Sy Duong-Quy. Vietnam Society of Sleep Medicine.
E-mail: sduongquy.jfvp@gmail.com
ABSTRACT
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality and is characterized by breathing impairment and related symptoms. Obstructive sleep apnoea (OSA) is strongly associated with COPD and is a highly prevalent condition that adversely affects breathing during sleep. The co-occurrence of OSA and COPD in an individual has been referred to the overlap syndrome (OVS). Patients with COPD and OSA may have more frequent and severe nocturnal arterial hypoxemia and hypercapnia than in patients with OSA alone, as well as increased pulmonary hypertension and dysrhythmia. The presence of OSA in patients with COPD has also been implicated as a risk factor for COPD exacerbations and associated hospitalizations. Patients with overlapping syndrome, when compared with patients with obstructive respiratory disease only, had a higher Epworth score, lower total sleep time, and sleep efficiency. Age, gender, BMI and the presence of co-morbidities such as hypertension may be superior beside the traditional symptoms of OSA. Continuous positive airway pressure (CPAP) therapy reduces the mortality rate in people who have both COPD and OSA. The co-occurrence of OSA and COPD is common condition with high number of patients. The clinical signs such as snoring, nocturia and daytime sleepiness (Epworth score) and PSG are required signs and very useful to detect OSA in COPD patients. The most effective treatment option for OSA is CPAP therapy, which helps keep the airway open by providing a stream of air through a mask that is worn during sleep.
KEYWORDS: OSA; COPD; AHI; Epworth; Overlap syndrome; CPAP.
RÉSUMÉ
La maladie pulmonaire obstructive chronique (MPOC) est une cause majeure de morbidité et de mortalité et se caractérise par des difficultés respiratoires et des symptômes associés. L'apnée obstructive du sommeil (AOS) est fortement associée à la BPCO et constitue une affection très répandue qui affecte négativement la respiration pendant le sommeil. La cooccurrence de l'AOS et de la BPCO chez un individu a été appelée syndrome de chevauchement (OVS). Les patients atteints de BPCO et d'AOS peuvent présenter une hypoxémie artérielle et une hypercapnie nocturnes plus fréquentes et plus graves que les patients atteints d'AOS seule, ainsi qu'une augmentation de l'hypertension pulmonaire et de la dysrythmie. La présence d'AOS chez les patients atteints de BPCO a également été impliquée comme facteur de risque d'exacerbations de BPCO et d'hospitalisations associées. Les patients présentant un syndrome de chevauchement, par rapport aux patients atteints uniquement d'une maladie respiratoire obstructive, présentaient un score d'Epworth plus élevé, une durée totale de sommeil et une efficacité du sommeil inférieures. L'âge, le sexe, l'IMC et la présence de comorbidités telles que l'hypertension peuvent être supérieurs aux symptômes traditionnels de l'AOS. La thérapie par pression positive continue (CPAP) réduit le taux de mortalité chez les personnes atteintes à la fois de BPCO et d'AOS. La cooccurrence de l’AOS et de la BPCO est une pathologie courante touchant un nombre élevé de patients. Les signes cliniques tels que le ronflement, la nycturie et la somnolence diurne (score d'Epworth) et la PSG sont des signes obligatoires et très utiles pour détecter l'AOS chez les patients BPCO. L’option de traitement la plus efficace contre l’AOS est la thérapie CPAP, qui aide à maintenir les voies respiratoires ouvertes en fournissant un flux d’air à travers un masque porté pendant le sommeil.
MOTS CLÉS: AOS; BPCO; AHI; Epworth; Syndrome de chevauchement; CPAP.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) affects about 10% of adults and obstructive sleep apnea (OSA) is also reported to have a similarly high incidence [15]. COPD and OSA are highly prevalent diseases and thus likely to coexist in the same patient; a disorder otherwise known as overlap syndrome (OS).[24][8] According to S Duong-Quy et al (2018): OSA has apnea - hypopnea index (AHI) > 5 found in 8.5% and AHI > 15 (5.2% of cases) [21]. A recent review by Shawon et al also concluded that the incidence of OVS ranged from 2.9% to 65.9% in patients with COPD [16]. OSA was associated with overall worse outcomes in patients with COPD. Clearly, there is an increasing demand to identify OSA among the COPD population. Scientists have already tried to explore associations between these two diseases, in terms of epidemiology, overlapping pathophysiology, shared risk factors, presence of other comorbidities, clinical outcomes, and optimal management [10].
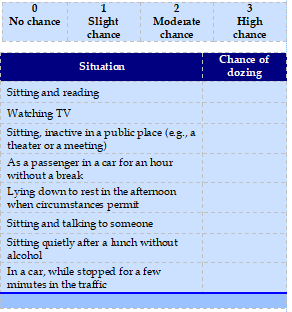
Surprisingly, body mass index (BMI) and smoking pack years, but not the Epworth Sleepiness Scale (ESS)' score, were found to be predictors of coexistent OSA in a group of COPD patients [19]. Moreover, increased risk for OSA in patients with COPD was related to higher scores in COPD Assessment Test and more prevalent cardiometabolic disease. In addition, the degree of airflow limitation is another issue to consider, as moderate-to-severe COPD is related to a high prevalence of OSA [17]. Of note, hyperinflation and emphysema are inversely correlated with the severity of OSA in COPD patients,[10] reinforcing the fact that the chronic bronchitis phenotype of COPD is strongly associated with OSA. In a landmark study [9], nontreated patients with OS carried a higher mortality and hospitalization risk compared to patients with COPD only.
PREVALENCE OF OSA AND COPD OVERLAP
More than three quarters of patients with COPD report nocturnal discomfort symptoms. Sleep complaints increase with more severe illness [6]. S Duong Quy reported that the prevalence of OSA in COPD patients is higher than in non-COPD group (23% versus 10%) and there was a significant correlation between AHI and snoring during sleep, nocturia and Epworth score (r = 0.614, p <0.05, r = 0.672, p <0.05, r = 0.526, p <0.01) [20]. The high prevalence of OSA in lower airway diseases (asthma, COPD and asthma-COPD overlap - ACO) was from 35.5% to 64.4%.
A study of Pavel Turcania (2014) noted that the OSA rate among COPD patients who hospitalized for acute exacerbations was 51.4% [14]. And if patient has a sustain increase in CO2, the OVS rate is up to 82% according to Cristina Miralles (2013).
PATHOPHYSIOLOGY OF OSA AND COPD OVERLAP
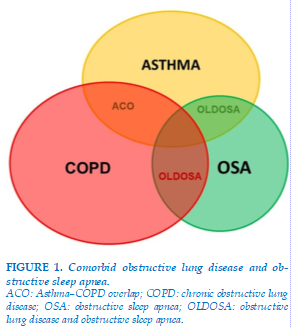
There is a decrease in blood oxygen saturation at night compared to COPD patients without OSA or OSA alone. Both COPD and OSA are associated with a range of overlapping physiological and biological disturbances that include hypoxia and inflammation, which likely contribute to cardiovascular and other comorbidities. Thus the probability is high that the overlap syndrome will be associated with a greater risk of comorbidity than is true with either disease alone. Actually, the risk of respiratory failure increase with higher CO2 and pulmonary hypertension although the bronchial obstruction is mild or moderate level. COPD has long been recognized to be associated with oxygen desaturation during sleep, which may exceed that associated with maximum. Figure 1 shows the overlap between asthma, COPD and OSA.
ACO: Asthma–COPD overlap; COPD: chronic obstructive lung disease; OSA: obstructive sleep apnea; OLDOSA: obstructive lung disease and obstructive sleep apnea.
Notably, OSA and COPD share common risk factors and pathophysiological mechanisms. Age, obesity, and tobacco exposure are well-recognized risk factors. Synergistically, both disorders are associated with systemic inflammation, oxidative stress, excitations in sympathetic activity, and endothelial dysfunction. Because OSA is characterized by intermittent whereas COPD by sustained hypoxia, impaired oxygenation during both wakefulness and sleep is observed in OSA, and it is more pronounced compared to COPD or OSA alone. These characteristics can increase the risk for the development, or progression of already-established in OSA.
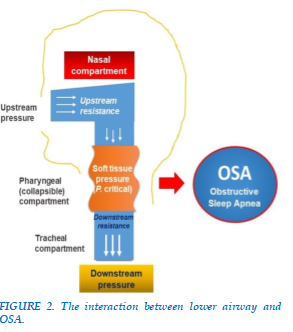
The model predicts the effects of transmural pressure on airflow dynamics and the severity of upper and lower airway obstruction during sleep as follows (Figure 2).
The epidemiological relationship of COPD and OSA are related different clinical phenotypes. Different clinical COPD phenotypes influence the likelihood of coexisting OSA in that the increased lung volumes and low BMI associated with the predominant emphysema phenotype protects against OSA, whereas the higher likelihood of peripheral edema and increased BMI associated with the predominant chronic bronchitis phenotype promotes OSA [11].
PATHOPHYSIOLOGY OF OSA AND COPD OVERLAP
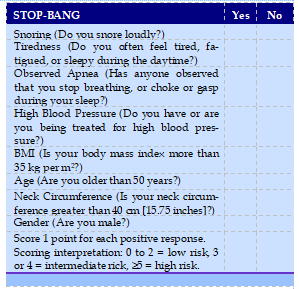
The diagnosis of OSA in patients with COPD requires awareness of relevant clinical features, and screening questionnaires may help identify suitable patients for further overnight study. Well-accepted screening tools for OSA are not always valid in COPD individuals [18]. Nevertheless, among them, the STOP-BANG questionnaire (SBQ) was found to be the most accurate [26]. Interestingly, BMI ≥25 kg/m2 and the presence of CVD perform better than other screening tools, such as the Epworth Sleepiness Scale (ESS) or the SBQ, in identifying OSA in COPD [18].
STOP-BANG questionnaire (Source: University Health Network, Toronto, Ontario, Canada (www.stobang.ca/osa/screening’php). Used with permission from Sauk Prairie Healthcare.
Whereas COPD can easily be diagnosed by spirometry, OSA diagnosis requires a sleep study, which is more expensive and time-consuming. Sleep physicians should choose between the gold standard polysomnography (PSG) and respiratory polygraphy. The diagnostic criteria for adult OSA as defined by the American Academy of Sleep Medicine (AASM)[1]. The patient suspected of OSAS must fulfill criterion A or B, plus criterion C. These are as follows:
A. Excessive daytime sleepiness that is not better explained by other factors
B. Two or more of the following that are not better explained by other factors:
C. Overnight monitoring demonstrates five or more obstructed breathing events per hour during sleep. These events may include any combination of obstructive apneas/hypopneas or respiratory effort–related arousals, as defined below.
They also proposed a grading of severity of OSAS based on the frequency of abnormal respiratory events during sleep: Mild: ≥ 5 but <15 events/hour of sleep; Moderate: 15–30 events/hour of sleep; Severe: More than 30 events/hour of sleep.
Effective treatment of OSA with the appropriate type of positive airway pressure (PAP) device is another matter of debate. Different strategy approaches should be applied to OSA patients with severe OSA and mild COPD than to those with mild OSA and severe COPD. Where OSA predominates, continuous PAP (CPAP) is the preferred modality, while bi-level PAP (BPAP) would be more appropriate when COPD prevails in OSA. Interestingly, the severity of nocturnal hypoxia and daytime hypercapnia in OS patients precludes the success of treatment with CPAP and shows that BPAP should be the first choice in such patients [7].
DIAGNOSIS APPROACH
The possibility that COPD may predispose to OSA and OSA to COPD has been explored in many studies over the past 2 decades. COPD and OSA are both highly prevalent, which implies that both disorders occurring together (OVS) is likely to be common based on chance association alone. Both COPD and OSA are associated with similar physiological and molecular consequences, such as hypoxia and systemic inflammation, that contribute to cardiovascular and other comorbidities, and pulmonary hypertension is highly prevalent in patients with the overlap syndrome [28-30].
Sleep quality is typically poor in COPD with diminished amounts of rapid eye movement (REM) and slow-wave sleep, which may contribute to the daytime fatigue frequently reported by these patients and may also contribute to reduced survival. A recent report has demonstrated that sleep impairment in COPD is linked to worse pulmonary function and lower daytime activity levels [12]. Lung hyperinflation also appears to relate to poor sleep quality in patients with COPD. In accordance with these findings, in this issue of this journal [12] the authors provide important evidence to support the screening of OSA in COPD patients with EDS. In this cross-sectional study, the authors assessed for the presence of EDS (based on ESS
score) in 301 stable COPD patients with severe and very severe airflow obstruction. Those with EDS (n = 47) underwent an attended PSG. A high prevalence of concurrent OSA in the subgroup of sleepy COPD participants was noted (70.2%), while the overall prevalence of OSA was approximately 10%. Of note, the selective evaluation with PSG of sleepy-only COPD patients, might have underestimated the true prevalence of OSA in this cohort. Collectively, these findings add significant evidence to the existing literature on predicting the risk of OSA and highlight the need for further research on this topic [8].
TREATMENT STRATEGY
Considering the fact that OSA is fully reversible after treatment, its diagnosis is highly important, as previous data has shown that in patients with OS treatment of OSA can improve COPD related outcomes and increase patients' survival [9]. COPD is not a uniform disease but represents a spectrum of clinical phenotypes. These range from the hyperinflated patient with low BMI who typically presents with predominant symptoms of dyspnea and relatively well preserved gas exchange (predominant emphysema phenotype) to the patient with higher BMI and cor pulmonale (right-sided heart failure) who typically presents with productive cough and hypoxemia (predominant chronic bronchitis phenotype) [31-34].
Objective sleep evaluation should be offered to all COPD patients, not only in the presence of well-known risk factors or symptoms of OSA [12], but whenever sleep-related issues are mentioned [2]. Indeed, accumulating evidence shows that OS patients typically complain of fatigue, whereas insomnia is also a salient feature of sleep-reported issues in COPD patients. Patients with the overlap syndrome will present with the clinical features of each disorder to a greater or lesser extent, depending on the balance between the COPD and OSA components. However, there are also likely to be additional clinical features to reflect the higher prevalence of hypoxemia, hypercapnia, and pulmonary hypertension.
Patients with COPD and nocturnal hypoxemia benefit from inhaled long-acting beta-agonist and anticholinergic therapy with the mean nocturnal oxygen saturation being about 2% to 3% higher on each medication compared with placebo. Both agents have no significant impact on sleep quality. Theophylline also reduces nocturnal hypoxemia and has been shown to benefit OSA by reducing the AHI. The recognition of coexisting OSA in patients with COPD has important clinical relevance, as the management of patients with overlap syndrome is different from the management of COPD alone, and the survival of patients with overlap syndrome that is not treated with nocturnal PAP is significantly inferior to that of patients with overlap syndrome that is appropriately treated.
CONCLUSION
The coexistence of OSA and COPD is common condition and increase medical burden than OSA or COPD alone. STOP-BANG and Epworth-score have screening implications for identifying patients with OVS and PSG are required signs and very useful to diagnose OSA in COPD patients. The most effective treatment option for OSA is CPAP therapy, which helps keep the airway open by providing a stream of air through a mask that is worn during sleep. Future research in this topic is needed so as to shed more light on the associations between OSA and COPD.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
DATA AVAILABILITY STATEMENT
This review did not have the raw data.
ETHICS STATEMENT
This review followed the Declaration of Helsinki – Ethical Principles for Medical Research involving human subjects.
AUTHOR CONTRIBUTIONS
D.NH, S.DQ, N.NTY, Q.DM, N.DT, B.LV, T.HA, Q.VTT, T.VPM , and V.NN: conceptualization, validation, and writing–original draft preparation. D.NH, S.DQ, N.NTY, T.VPM, and V.NN: methodology and writing–review and editing. All authors contributed to the article and approved the submitted version.
REFERENCES
| 1. American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 1999;22:667–689. |
| 2. Budhiraja R, Siddiqi TA, Quan SF. Sleep disorders in chronic obstructive pulmonary disease: Etiology, impact, and management. J Clin Sleep Med. 2015;11:259–70. |
| 3. Hang LW, Hsu JY, Chang CJ, Wang HC, Cheng SL, Lin CH, et al. Predictive factors warrant screening for obstructive sleep apnea in COPD: A Taiwan national survey. Int J Chron Obstruct Pulmon Dis. 2016;11:665–73. |
| 4. Johns Murray W. (1991), "A New Method for Measuring Daytime Sleepiness: The Epworth Sleepiness Scale ", Sleep, 14(6), pp. 540-545. |
| 5. Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017 ar 15;13(3):479-504 |
| 6. Katherine A. Dudley, MD, Atul Malhotra, MD, and Robert L. Owens, MD. Pulmonary Overlap Syndromes, with a focus on COPD and ILD. Sleep Med Clin. 2014 Sep; 9(3): 365–379. |
| 7. Kuklisova Z, Tkacova R, Joppa P, Wouters E, Sastry M. Severity of nocturnal hypoxia and daytime hypercapnia predicts CPAP failure in patients with COPD and obstructive sleep apnea overlap syndrome. Sleep Med. 2017;30:139–45. |
| 8. Malhotra A, Schwartz AR, Schneider H, Owens RL, DeYoung P, Han MK, et al. Research priorities in pathophysiology for sleep-disordered breathing in patients with chronic obstructive pulmonary disease. An official American thoracic society research statement. Am J Respir Crit Care Med. 2018;197:289–99. |
| 9. Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: The overlap syndrome. Am J Respir Crit Care Med. 2010;182:325–31. |
| 10. McNicholas WT. COPD-OSA overlap syndrome: Evolving evidence regarding epidemiology, clinical consequences, and management. Chest. 2017;152:1318–26. |
| 11. McNicholas WT. Bidirectional relationships of comorbidity with obstructive sleep apnoea. European Respiratory Review 2022 31: 210256. |
| 12. Nattusami L, Hadda V, Khilnani GC, Madan K, Mittal S, Tiwari P, et al. Co-existing obstructive sleep apnea among patients with chronic obstructive pulmonary disease. Lung India. 2021;38:12–7. |
| 13. Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of Adult Obstructive Sleep Apnea with Positive Airway Pressure: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2019 Feb 15;15(2):335-343. |
| 14. Pavel Turcania,b, Jana Skrickovab,c, Tomas Pavlikc, Eva Janousovac, Marek Orbana. The prevalence of obstructive sleep apnea in patients hospitalized for COPD exacerbation. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014; 158. |
| 15. Sharma B, Feinsilver S, Owens RL, Malhotra A, McSharry D, Karbowitz S. Obstructive airway disease and obstructive sleep apnea: Effect of pulmonary function. Lung. 2011; 189 (1):37–41.[PubMed]. |
| 16. Shawon M S, Perret J L, Senaratna C V, Lodge C, et al, (2017), "Current evidence on prevalence and clinical outcomes of co-morbid obstructive sleep apnea and chronic obstructive pulmonary disease: A systematic review", Sleep Med Rev, 32 pp. 58-68. |
| 17. Soler X, Gaio E, Powell FL, Ramsdell JW, Loredo JS, Malhotra A, et al. High prevalence of obstructive sleep apnea in patients with moderate to severe chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2015;12:1219–25. |
| 18. Soler X, Liao S-Y, Marin JM, Lorenzi-Filho G, Jen R, DeYoung P, et al. Age, gender, neck circumference, and Epworth sleepiness scale do not predict obstructive sleep apnea (OSA) in moderate to severe chronic obstructive pulmonary disease (COPD): The challenge to predict OSA in advanced COPD. PLoS ONE. 2017;12:e0177289. |
| 19. Steveling EH, Clarenbach CF, Miedinger D, Enz C, Dürr S, Maier S, et al. Predictors of the overlap syndrome and its association with comorbidities in patients with chronic obstructive pulmonary disease. Respiration. 2014;88:451–7. |
| 20. S Duong-Quy (2013). Étude des caractéristiques du syndrome d’apnées obstructives chez les patients atteints de BPCO. J Func Vent Pulm 2013. 04(11), 1- 52. |
| 21. S Duong-Quy, K Thi Mai Dang, N Van Tran, H Xuan Bich Nguyen, T Hua-Huy, F Chalumeau, AT DinhXuan, F Soyez, F Martin (2018). Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam. Revue des maladies respiratoires 35: 14-24. |
| 22. Voulgaris A, Nena E, Steiropoulos P. Comment on: Comorbidities in coexisting chronic obstructive pulmonary disease and obstructive sleep apnea-overlap syndrome. Eur Rev Med Pharmacol Sci. 2018;22:6171–2. |
| 23. Voulgaris A, Archontogeorgis K, Papanas N, Pilitsi E, Nena E, Xanthoudaki M, et al. Increased risk for cardiovascular disease in patients with obstructive sleep apnoea syndrome-chronic obstructive pulmonary disease (overlap syndrome) Clin Respir J. 2019;13:708–15. |
| 24. Voulgaris A, Archontogeorgis K, Steiropoulos P, Papanas N. Cardiovascular disease in patients with chronic obstructive pulmonary disease, obstructive sleep apnoea syndrome and overlap syndrome. Curr Vasc Pharmacol. 2020 . |
| 25. Voulgaris A, Steiropoulos P. Coexistent obstructive sleep apnea in patients with chronic obstructive pulmonary disease: Several unanswered questions need to be addressed. Lung India. 2021 Mar-Apr; 38(2): 191–192. |
| 26. Xiong M, Hu W, Dong M, Wang M, Chen J, Xiong H, et al. The screening value of ESS, SACS, BQ, And SBQ on obstructive sleep apnea in patients with chronic obstructive pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2019;14:2497–505. |
| 27. Duong-Quy S, Nguyen-Huu H, Hoang-Chau-Bao D, Tran-Duc S, Nguyen-Thi-Hong L, Nguyen-Duy T, Tang-Thi-Thao T, Phan C, Bui-Diem K, Vu-Tran-Thien Q, Nguyen-Ngoc-Phuong T, Nguyen-Nhu V, Le-Thi-Minh H, Craig T. Personalized Medicine and Obstructive Sleep Apnea. Journal of Personalized Medicine. 2022; 12(12):2034. https://doi.org/10.3390/jpm12122034 |
| 28. Duong-Quy, S., Hua-Huy, T., Tran-Mai-Thi, H. T., Le-Dong, N. N., Craig, T. J., & Dinh-Xuan, A. T. (2016). Study of Exhaled Nitric Oxide in Subjects with Suspected Obstructive Sleep Apnea: A Pilot Study in Vietnam. Pulmonary Medicine, 2016, 21-27. |
| 29. Hua-Huy, T., Le-Dong, N. N., Duong-Quy, S., Luchon, L., Rouhani, S., & Dinh-Xuan, A. T. (2015). Increased alveolar nitric oxide concentration is related to nocturnal oxygen desaturation in obstructive sleep apnoea. Nitric Oxide, 45, 27-34. |
| 30. Duong-Quy, S., Hua-Huy, T., Mai-Huu-Thanh, B., Doan-Thi-Quynh, N., Le-Quang, K., Nguyen-Van, H., ... & Homasson, J. P. (2009). Early detection of smoking related chronic obstructive pulmonary disease in Vietnam. Revue des maladies respiratoires, 26(3), 267-274. |
| 31. Duong-Quy, S., Tran Van, H., Vo Thi Kim, A., Pham Huy, Q., & Craig, T. J. (2018). Clinical and functional characteristics of subjects with asthma, COPD, and asthma-COPD overlap: A multicentre study in Vietnam. Canadian Respiratory Journal, 2018. |
| 32. Vo-Thi-Kim, A., Van-Quang, T., Nguyen-Thanh, B., Dao-Van, D., & Duong-Quy, S. (2020). The effect of medical treatment on nasal exhaled nitric oxide (NO) in patients with persistent allergic rhinitis: A randomized control study. Advances in medical sciences, 65(1), 182-188. |
| 33. Duong-Quy, S., Vo-Pham-Minh, T., Duong-Thi-Thanh, V., Craig, T., & Nguyen-Nhu, V. (2023). Clinical Approaches to Minimize Readmissions of Patients with COPD: A Narrative Review. Current Respiratory Medicine Reviews, 19(1), 12-23. |
| 34. Dang-Thi-Mai, K., Le-Dong, N. N., Bui-Diem, K., Vu-Tran-Thien, Q., Nguyen-Nhu, V., & Duong-Quy, S. (2021). Exhaled Nitric Oxide as a Potential Biomarker of Continuous Positive Airway Pressure Therapy for Severe Obstructive Sleep Apnea Patients. Current Respiratory Medicine Reviews, 17(3), 192-198. |
TABLE - FIGURES
REFERENCES
| 1. American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 1999;22:667–689. |
| 2. Budhiraja R, Siddiqi TA, Quan SF. Sleep disorders in chronic obstructive pulmonary disease: Etiology, impact, and management. J Clin Sleep Med. 2015;11:259–70. |
| 3. Hang LW, Hsu JY, Chang CJ, Wang HC, Cheng SL, Lin CH, et al. Predictive factors warrant screening for obstructive sleep apnea in COPD: A Taiwan national survey. Int J Chron Obstruct Pulmon Dis. 2016;11:665–73. |
| 4. Johns Murray W. (1991), "A New Method for Measuring Daytime Sleepiness: The Epworth Sleepiness Scale ", Sleep, 14(6), pp. 540-545. |
| 5. Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017 ar 15;13(3):479-504 |
| 6. Katherine A. Dudley, MD, Atul Malhotra, MD, and Robert L. Owens, MD. Pulmonary Overlap Syndromes, with a focus on COPD and ILD. Sleep Med Clin. 2014 Sep; 9(3): 365–379. |
| 7. Kuklisova Z, Tkacova R, Joppa P, Wouters E, Sastry M. Severity of nocturnal hypoxia and daytime hypercapnia predicts CPAP failure in patients with COPD and obstructive sleep apnea overlap syndrome. Sleep Med. 2017;30:139–45. |
| 8. Malhotra A, Schwartz AR, Schneider H, Owens RL, DeYoung P, Han MK, et al. Research priorities in pathophysiology for sleep-disordered breathing in patients with chronic obstructive pulmonary disease. An official American thoracic society research statement. Am J Respir Crit Care Med. 2018;197:289–99. |
| 9. Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: The overlap syndrome. Am J Respir Crit Care Med. 2010;182:325–31. |
| 10. McNicholas WT. COPD-OSA overlap syndrome: Evolving evidence regarding epidemiology, clinical consequences, and management. Chest. 2017;152:1318–26. |
| 11. McNicholas WT. Bidirectional relationships of comorbidity with obstructive sleep apnoea. European Respiratory Review 2022 31: 210256. |
| 12. Nattusami L, Hadda V, Khilnani GC, Madan K, Mittal S, Tiwari P, et al. Co-existing obstructive sleep apnea among patients with chronic obstructive pulmonary disease. Lung India. 2021;38:12–7. |
| 13. Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of Adult Obstructive Sleep Apnea with Positive Airway Pressure: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2019 Feb 15;15(2):335-343. |
| 14. Pavel Turcania,b, Jana Skrickovab,c, Tomas Pavlikc, Eva Janousovac, Marek Orbana. The prevalence of obstructive sleep apnea in patients hospitalized for COPD exacerbation. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014; 158. |
| 15. Sharma B, Feinsilver S, Owens RL, Malhotra A, McSharry D, Karbowitz S. Obstructive airway disease and obstructive sleep apnea: Effect of pulmonary function. Lung. 2011; 189 (1):37–41.[PubMed]. |
| 16. Shawon M S, Perret J L, Senaratna C V, Lodge C, et al, (2017), "Current evidence on prevalence and clinical outcomes of co-morbid obstructive sleep apnea and chronic obstructive pulmonary disease: A systematic review", Sleep Med Rev, 32 pp. 58-68. |
| 17. Soler X, Gaio E, Powell FL, Ramsdell JW, Loredo JS, Malhotra A, et al. High prevalence of obstructive sleep apnea in patients with moderate to severe chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2015;12:1219–25. |
| 18. Soler X, Liao S-Y, Marin JM, Lorenzi-Filho G, Jen R, DeYoung P, et al. Age, gender, neck circumference, and Epworth sleepiness scale do not predict obstructive sleep apnea (OSA) in moderate to severe chronic obstructive pulmonary disease (COPD): The challenge to predict OSA in advanced COPD. PLoS ONE. 2017;12:e0177289. |
| 19. Steveling EH, Clarenbach CF, Miedinger D, Enz C, Dürr S, Maier S, et al. Predictors of the overlap syndrome and its association with comorbidities in patients with chronic obstructive pulmonary disease. Respiration. 2014;88:451–7. |
| 20. S Duong-Quy (2013). Étude des caractéristiques du syndrome d’apnées obstructives chez les patients atteints de BPCO. J Func Vent Pulm 2013. 04(11), 1- 52. |
| 21. S Duong-Quy, K Thi Mai Dang, N Van Tran, H Xuan Bich Nguyen, T Hua-Huy, F Chalumeau, AT DinhXuan, F Soyez, F Martin (2018). Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam. Revue des maladies respiratoires 35: 14-24. |
| 22. Voulgaris A, Nena E, Steiropoulos P. Comment on: Comorbidities in coexisting chronic obstructive pulmonary disease and obstructive sleep apnea-overlap syndrome. Eur Rev Med Pharmacol Sci. 2018;22:6171–2. |
| 23. Voulgaris A, Archontogeorgis K, Papanas N, Pilitsi E, Nena E, Xanthoudaki M, et al. Increased risk for cardiovascular disease in patients with obstructive sleep apnoea syndrome-chronic obstructive pulmonary disease (overlap syndrome) Clin Respir J. 2019;13:708–15. |
| 24. Voulgaris A, Archontogeorgis K, Steiropoulos P, Papanas N. Cardiovascular disease in patients with chronic obstructive pulmonary disease, obstructive sleep apnoea syndrome and overlap syndrome. Curr Vasc Pharmacol. 2020 . |
| 25. Voulgaris A, Steiropoulos P. Coexistent obstructive sleep apnea in patients with chronic obstructive pulmonary disease: Several unanswered questions need to be addressed. Lung India. 2021 Mar-Apr; 38(2): 191–192. |
| 26. Xiong M, Hu W, Dong M, Wang M, Chen J, Xiong H, et al. The screening value of ESS, SACS, BQ, And SBQ on obstructive sleep apnea in patients with chronic obstructive pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2019;14:2497–505. |
| 27. Duong-Quy S, Nguyen-Huu H, Hoang-Chau-Bao D, Tran-Duc S, Nguyen-Thi-Hong L, Nguyen-Duy T, Tang-Thi-Thao T, Phan C, Bui-Diem K, Vu-Tran-Thien Q, Nguyen-Ngoc-Phuong T, Nguyen-Nhu V, Le-Thi-Minh H, Craig T. Personalized Medicine and Obstructive Sleep Apnea. Journal of Personalized Medicine. 2022; 12(12):2034. https://doi.org/10.3390/jpm12122034 |
| 28. Duong-Quy, S., Hua-Huy, T., Tran-Mai-Thi, H. T., Le-Dong, N. N., Craig, T. J., & Dinh-Xuan, A. T. (2016). Study of Exhaled Nitric Oxide in Subjects with Suspected Obstructive Sleep Apnea: A Pilot Study in Vietnam. Pulmonary Medicine, 2016, 21-27. |
| 29. Hua-Huy, T., Le-Dong, N. N., Duong-Quy, S., Luchon, L., Rouhani, S., & Dinh-Xuan, A. T. (2015). Increased alveolar nitric oxide concentration is related to nocturnal oxygen desaturation in obstructive sleep apnoea. Nitric Oxide, 45, 27-34. |
| 30. Duong-Quy, S., Hua-Huy, T., Mai-Huu-Thanh, B., Doan-Thi-Quynh, N., Le-Quang, K., Nguyen-Van, H., ... & Homasson, J. P. (2009). Early detection of smoking related chronic obstructive pulmonary disease in Vietnam. Revue des maladies respiratoires, 26(3), 267-274. |
| 31. Duong-Quy, S., Tran Van, H., Vo Thi Kim, A., Pham Huy, Q., & Craig, T. J. (2018). Clinical and functional characteristics of subjects with asthma, COPD, and asthma-COPD overlap: A multicentre study in Vietnam. Canadian Respiratory Journal, 2018. |
| 32. Vo-Thi-Kim, A., Van-Quang, T., Nguyen-Thanh, B., Dao-Van, D., & Duong-Quy, S. (2020). The effect of medical treatment on nasal exhaled nitric oxide (NO) in patients with persistent allergic rhinitis: A randomized control study. Advances in medical sciences, 65(1), 182-188. |
| 33. Duong-Quy, S., Vo-Pham-Minh, T., Duong-Thi-Thanh, V., Craig, T., & Nguyen-Nhu, V. (2023). Clinical Approaches to Minimize Readmissions of Patients with COPD: A Narrative Review. Current Respiratory Medicine Reviews, 19(1), 12-23. |
| 34. Dang-Thi-Mai, K., Le-Dong, N. N., Bui-Diem, K., Vu-Tran-Thien, Q., Nguyen-Nhu, V., & Duong-Quy, S. (2021). Exhaled Nitric Oxide as a Potential Biomarker of Continuous Positive Airway Pressure Therapy for Severe Obstructive Sleep Apnea Patients. Current Respiratory Medicine Reviews, 17(3), 192-198. |
ARTICLE INFO DOI: 10.12699/jfvpulm.15.46.2024.01
Conflict of Interest
Non
Date of manuscript receiving
22/01/2024
Date of publication after correction
22/04/2024
Article citation
Duc Nguyen-Hong, Nhi Nguyen-Thi-Y, Quy Duong-Minh, Nghia Dam-Trung, Bang Le-Van, Sy Duong-Quy. Diagnosis and management of obstructive sleep apnea in patients with chronic obstructive pulmonary disease. J Func Vent Pulm 2024;46(15):1-6