
 English
English
 French
French
Transverse myelitis: A rare neurological complication of tuberculosis
Myélite transverse: Une complication neurologique rare de la tuberculose
Mohamed Amine Mnaili1,2 Ahmed Bourazza3
1: Neurology departement, Agadir Military Hospital, Agadir, Morocco
2: University of Hassan II, Casablanca, Morocco
3: Neurology departement, Mohammed V Military Hospital, Rabat, Morocco
Corresponding author:
MNAILI Mohamed Amine. Neurology departement, Agadir Military Hospital, Agadir, Morocco.
E-mail: aminemed08@gmail.com
ABSTRACT
Acute transverse myelitis is a rare inflammatory demyelinating disorder characterized by relatively acute onset of motor, sensory, and autonomic dysfunction. Mycobacterium tuberculosis is a very rare cause of transverse myelitis. We present a patient with tuberculosis presenting with meningitis and transverse myelitis who had marked clinical improvement and neurologic recovery after treatment of tuberculosis and intravenous steroid pulses.
Acute transverse myelitis is a rare inflammatory demyelinating disorder characterized by the relatively acute onset of motor, sensory, and autonomic dysfunction. Mycobacterium tuberculosis is a very rare cause of transverse myelitis. We present a tuberculosis patient with meningitis and transverse myelitis who showed marked clinical improvement and neurological recovery after treatment of tuberculosis and intravenous steroid pulses.
KEYWORDS: Tuberculosis; Neurological tuberculosis; Transverse myelitis.
RÉSUMÉ
La myélite transverse aiguë est un trouble démyélinisant inflammatoire rare caractérisé par l'apparition relativement aiguë d'un dysfonctionnement moteur, sensoriel et autonome. Mycobacterium tuberculosis est une cause très rare de myélite transverse. Nous présentons un patient atteint de tuberculose présentant une méningite et une myélite transverse qui présentait une amélioration clinique marquée et une récupération neurologique après le traitement de la tuberculose et des impulsions de stéroïdes intraveineuses.
La myélite transverse aiguë est un trouble démyélinisant inflammatoire rare caractérisé par l'apparition relativement aiguë d'un dysfonctionnement moteur, sensoriel et autonome. Mycobacterium tuberculosis est une cause très rare de myélite transverse. Nous présentons un patient de tuberculose présentant une méningite et une myélite transverse qui présentait une clinique marquée et une récupération neurologique après le traitement de la tuberculose et des impulsions de stéroïdes intraveineuses.
MOTS CLÉS: Tuberculose; tuberculose neurologique; myélite transverse.
INTRODUCTION
Longitudinally extensive transverse myelitis (LETM) is characterized by contiguous inflammatory lesions of spinal cord extending to ≥3 vertebral segments [1]. The causes of LETM including various infections, neoplastic reason, and autoimmune disease [2]. Neuromyelitis optica spectrum disorder (NMOSD) is the most common cause of LETM. Of all cases of tuberculosis, central nervous system is affected in approximately 1%, with spinal cord involvement seen in less than half of these cases, with a higher prevalence for HIV infected individuals [3]. Most often, central nervous system tuberculosis pertains to tuberculous meningitis (95%), space-occupying cerebral or medular tuberculoma, and radiculomyelitis, and very rarely to longitudinally extensive transverse myelitis (LETM) [4]. Cases of transverse myelitis associated with TB are very rare or usually not reported. Cerebrospinal fluid analysis and magnetic resonance imaging of spinal cord plus bacteriological confirmation of tuberculous infection are necessary for the diagnosis. We report a case-patient with TB presenting with meningitis and transverse myelitis who had achieved clinical improvement and complete neurologic recovery after empirical anti-tubercular treatment and high doses of systemic corticosteroids.
CASE REPORT
A 32-year-old male, with no past medical history but a nephew recently diagnosed with tuberculosis presented with 3 months of non-productive cough. By history there was also unquantified weight loss, asthenia, intermittent fever and night sweats. Two weeks before admission he had exacerbation of fever, severe headache, lower limb weakness, paresthesia and urinary retention. His family medical history was significant for pulmonary tuberculosis on his father’s side, for which he had received treatment 10 years ago. On physical examination, the patient was alert, oriented to person, place and time. Aside from urinary retention that needed indwelling catheter placement, the rest of the clinical examination of the genitourinary, respiratory, cardiovascular, and musculoskeletal systems was otherwise unremarkable. Neurological examination showed neck stiffness, positive Bruzinski and Kernig’s signs, arreflectic lower limbs, paraparesis in both lower limbs (strength 0/5 according to the Medical Research Council grade), and a positive Babinski sign. No visual disturbances were clear. Examination of the cranial nerves, cerebellum, cortical function, and upper extremities was within normal limits.
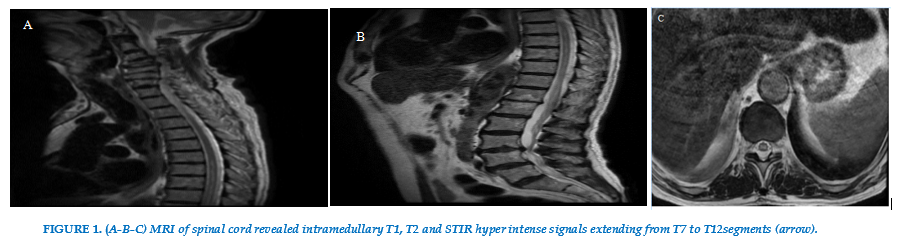
Spinal cord MRI revealed intramedullary T1, T2 and STIR hyper intense signals extending from T7 to T12 segments; confirming the suspicion of transversal
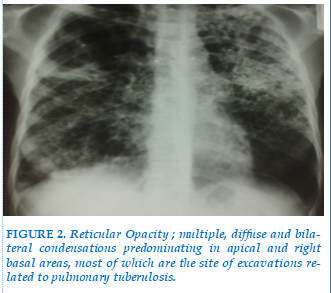
myelitis. Routine blood tests were normal. HIV and VDRL serologies were negative. Chest X-ray showed evidence reticular Opacity and multiple, diffuse and bilateral condensations related to pulmonary tuberulosis.
Considering the findings we performed a lumbar puncture. The cerebral spinal fluid analysis showed 39 white blood cells count/ mm3 with 15.4% lymphocytes and 84.6% neutrophils, elevated proteins (95 mg/dl), and a CSF glucose of 57 mg/dl (blood glucose 154 mg/dl), with normal opening pressure. Ziehl Nielssen stains were negative, as well as the Gram stains.
The clinical and MR findings were consistent with longitudinally extensive transverse myelitis, so a thorough work-up was performed for possible causes of LETM, testing for a series of markers of autoimmune disorders. ANA, DNA-ds as well as CSF angiotensin converting enzyme were found to be negative.
A combination of corticosteroid and antituberculosis treatment (isonicotinyl hydrazide 0.3 g/d, rifampin 0.45 g/d, pyrazinamide 1 g/d, ethambutol 1 g/d, and dexamethasone 15mg/d) was given. Neurological dysfunction was ameliorated significantly. The lesion size in the spinal cord and in the lung were significantly reduced 1 month later after discharge from the hospital. The EDSS of the patient dropped to 0 at the follow up time when 3 months after discharge from the hospital. (FIGURE 1). (FIGURE 2).
DISCUSSION
Mycobacterium tuberculosis is an acid fast pathogenic bacterium that primarily involves the lungs giving rise to tuberculosis. In developed countries the incidence of tuberculosis decreased in the past decades, but in countries with a lower standard of life, the disease is still a very serious health problem, being one of the front rank causes of infection related mortality and morbidity [5].
The main etiologic mechanism is thought to be an abnormal activation of the immune system against the spinal cord. This is thought to be a result of molecular mimicry phenomenon due to a similar subtype of ganglions that can be found in the cell wall of the human nervous tissue and on the cell wall of mycobacterium tuberculosis.The immune cells activated to fight off the infection, mistakenly also attack the neuronal cells, causing inflammation in the spinal cord. This inflammation leads to demyelination and neuronal injury of various degrees [6,7]. Another immune mediated mechanism is thought to be due to the superantigens that Mycobacterium tuberculosis has, which stimulate the activation of T cells to attack myelin proteins [8]. Other suspected mechanisms are the direct invasion by the bacillus. The disease begins with the development of small tuberculous foci (Rich foci) in the brain, spinal cord, or meninges. They can have a compressive effect on the spinal cord or can be present as intramedullary lesions.The location ofthese foci and the ability to control them ultimately determine which form of CNS tuberculosis occurs [9]. Transverse myelitis may also be due to vascular thrombosis or mechanisms related to the toxic effect of antituberculosis drugs [10].
TM is a rare neurological disorder characterized by an involvement of the spinal cord, due to acute inflammation that may evolve into cord ischemia and finally necrosis. It has an incidence between 1.34 and 4.6 per million per year, with bimodal peaks between ages 10–19 and 30–39 years [11]. The symptoms of TM usually progress over hours to few weeks. The most common symptoms include: lower limb paresthesia (80–95%), partial inability to move legs (paraparesia 50%), sensory level (80%), and bladder symptoms (almost 100%) [12]. Autonomic symptoms include urinary incontinence, as happened in the present case.
MRI of the spine is an important diagnostic tool in diagnosing TB myelopathy associated with longitudinally extensive lesion [13]. In addition to imaging, CSF studies play an important role in the diagnosis. In cases of TB myelopathy associated with longitudinally extensive lesion, a CSF analysis shows pleocytosis and increased protein levels, with normal glucose and opening pressures. Like our patient [14].There is no specific guideline at present for the treatment regime to apply to patients with TB myelopathy associated with longitudinally extensive lesion. Previous reports have considered a combination of steroid and antitubercular therapy to be appropriate. Antiretroviral therapy may be added to the treatment regime for patients with HIV [15,16].
CONCLUSION
Tuberculous transversal myelitis is rare but should be considered in the differential diagnosis of non-compressive myelopathies, particularly in the presence of pulmonary lesions in high burden TB countries or in the presence of clinical symptoms suggestive of TB. Appropriate knowledge about the clinical presentation and radiological and CSF findings is vital to ensuring an early and accurate diagnosis and hence the instigation of appropriate therapy.
CONFLICT OF INTEREST
None
REFERENCES
FIGURES
REFERENCES
ARTICLE INFO DOI: 10.12699/jfvpulm.15.46.2024.71
Conflict of Interest
Non
Date of manuscript receiving
25/03/2024
Date of publication after correction
26/06/2024
Article citation
Mohamed Amine Mnaili Ahmed Bourazza. Transverse myelitis: A rare neurological complication of tuberculosis. J Func Vent Pulm 2024;46(15):71-74