
 English
English
 French
French
Association between parasomnias and children with attention deficit hyperactivity disorder: A cross-sectional study in Vietnam
Association entre les parasomnies et les enfants atteints de trouble du déficit de l’attention avec hyperactivité: Une étude transversale au Vietnam
Mai Nguyen-Thi-Phuong¹, Mai Nguyen-Thi-Thanh¹, Sy Duong-Quy2,3,4
1Hanoi Medical University, Hanoi, Vietnam
2Sleep Lab Center of Vietnam Society of Sleep Medicine. Dalat, Vietnam
3Bio-Medical Research Center. Lam Dong Medical College. Dalat, Vietnam
4Hershey Medical Center. Penn State Medical College. PA, USA
Corresponding author: Mai Nguyen-Thi-Phuong. Hanoi Medical University, Hanoi, Vietnam
Email: nguyenthiphuongmai@hmu.edu.vn
ABSTRACT
Background. Attention deficit hyperactivity disorder (ADHD) is frequently associated with sleep disturbances, including parasomnias, which may worsen ADHD symptoms. However, the relationship between ADHD and parasomnias remains underexplored, particularly in newly diagnosed pediatric populations.
Objectives. This study aimed to determine the prevalence of parasomnias and identify associated factors in children with ADHD.
Methods. A cross-sectional study was conducted on 629 children aged 6 – 12 years newly diagnosed with ADHD according to DSM-5 criteria at Vietnam National Children's Hospital. Parasomnias were classified using the ICSD-3, and data on comorbidities and sleep behaviors were collected through structured interviews and sleep diaries. Univariate and multivariate logistic regression analyses were performed to determine significant associations.
Results. Parasomnias were identified in 27.8% of children with ADHD, with NREM-related parasomnias being the most prevalent. The presence of comorbid psychiatric disorders, particularly tic disorders, anxiety–depression, learning disorders, and intellectual disability, significantly increased parasomnia risk (OR 2.49 – 4.29, p < 0.001). Sleep talking was the strongest independent predictor (OR = 5.74, p < 0.001). ADHD clinical subtypes were not significantly associated with parasomnias.
Conclusion. Parasomnias are common in children with ADHD and are strongly linked to comorbid conditions and sleep-related behaviors. These findings emphasize the need for routine sleep assessments in ADHD management.
KEYWORDS: ADHD; Parasomnias; Sleep disorders; Comorbidities; Pediatric sleep; ICSD-3
RÉSUMÉ
Contexte. Le trouble du déficit de l’attention avec hyperactivité (TDAH) est souvent associé à des troubles du sommeil, notamment les parasomnies, pouvant aggraver les symptômes. La relation entre TDAH et parasomnies reste peu explorée, surtout chez les enfants récemment diagnostiqués.
Objectif. Déterminer la prévalence des parasomnies et leurs facteurs associés chez les enfants atteints de TDAH.
Méthodes. Étude transversale menée auprès de 629 enfants de 6 à 12 ans, nouvellement diagnostiqués avec un TDAH selon le DSM-5. Les parasomnies ont été identifiées selon l’ICSD-3, et les données ont été recueillies via entretiens structurés et journaux de sommeil. Des analyses statistiques ont été effectuées pour évaluer les associations.
Résultats. 27,8 % des enfants présentaient des parasomnies, principalement de type NREM. Les troubles psychiatriques comorbides (tics, anxiété-dépression, troubles de l’apprentissage, retard intellectuel) étaient des facteurs de risque importants. Le parler en dormant était le prédicteur le plus fort. Aucun lien significatif n’a été observé avec les sous-types cliniques du TDAH.
Conclusion. Les parasomnies sont fréquentes chez les enfants atteints de TDAH et sont liées aux comorbidités et comportements liés au sommeil. Une évaluation du sommeil devrait faire partie intégrante de la prise en charge du TDAH.
MOTS CLÉS: TDAH; Parasomnies; Troubles du sommeil; Comorbidités; Sommeil pédiatrique; ICSD-3
INTRODUCTION
La Attention deficit hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders in children, characterized by persistent symptoms of inattention, hyperactivity, and impulsivity that interfere with social, academic, and emotional functioning. Globally, the prevalence of ADHD is estimated at 5 – 7% among school-aged children, with a rising trend in diagnosis and research focus in recent years.[1]
Sleep disturbances are highly prevalent in children with ADHD, affecting up to 50 – 80% of cases.[2,3]Among these, parasomnias—undesirable physical events or experiences during sleep or sleep-wake transitions, have gained increasing attention due to their potential role in exacerbating ADHD symptoms. Parasomnias are classified into non-rapid eye movement (NREM)-related disturbances such as sleepwalking, sleep terrors, and confusional arousals, and rapid eye movement (REM)-related disturbances such as nightmares.[4,5]These episodes are often accompanied by autonomic arousal, behavioral dysregulation, and fragmented sleep, which may worsen daytime functioning in children with ADHD.[6]
The association between ADHD and parasomnias is believed to be bidirectional and multifactorial. Children with ADHD may have underlying sleep architecture abnormalities, impaired arousal mechanisms, or emotional dysregulation that predispose them to parasomnias.[7] Conversely, disrupted sleep from parasomnias can lead to increased irritability, inattention, and impulsivity during the day-mimicking or aggravating ADHD symptoms.[8] In addition, comorbid psychiatric conditions such as anxiety, depression, tic disorders, and autism spectrum disorder have been shown to increase the risk of sleep disturbances in this population.[9]
Despite the growing recognition of this interplay, few studies have comprehensively examined parasomnias and their associated factors in newly diagnosed pediatric ADHD populations, particularly in low- and middle-income countries. Cultural, environmental, and health system differences may further shape the presentation and impact of these disorders.[10]
This study aims to investigate the prevalence and associated factors of parasomnias in Vietnamese children with ADHD, contributing to a more integrated understanding of sleep and neurobehavioral health, and emphasizing the importance of routine sleep screening in ADHD assessment and management.
METHODS
Study Design and Participants
This cross-sectional descriptive study was conducted at the Department of Psychiatry, Vietnam National Children's Hospital, from October 1, 2022, to
September 30, 2024. A total of 629 children aged 6 to 12 years, newly diagnosed with ADHD based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria,[11] were consecutively recruited. Children were excluded if they had acute illnesses requiring hospitalization, chronic or malignant diseases (e.g., epilepsy, systemic lupus erythematosus, cancer), or if they were taking sedatives or medications known to affect sleep. Participants were also excluded if they or their caregivers did not consent, failed to follow study protocols, or did not provide sufficient information.
Diagnosis of Parasomnias
Sleep disorders were classified according to the International Classification of Sleep Disorders – Third Edition (ICSD-3). [4] Parasomnias were subdivided into NREM-related (e.g., sleepwalking, sleep terrors, confusional arousals) and REM-related parasomnias (e.g., nightmares). Diagnostic criteria followed ICSD-3 standards, which include recurrent episodes of incomplete awakening, inappropriate or absent response to external stimuli, limited recall, and exclusion of other sleep, medical, or substance-related disorders.[4]
Data Collection and Measurements
Data were collected through structured interviews with caregivers, medical records, and standardized sleep behavior questionnaires. A two-week sleep diary was completed by caregivers to document pre-sleep routines, nighttime awakenings, and post-sleep behaviors, allowing for comprehensive assessment of sleep environment and sleep hygiene factors.
Anthropometric data, physical comorbidities (e.g., allergic rhinitis, asthma, iron-deficiency anemia), ADHD subtypes, psychiatric comorbidities (e.g., learning disorders, tic disorders, anxiety-depression), and sleep-related behaviors were recorded.
Statistical Analysis
Categorical variables were expressed as frequencies and percentages; continuous variables were reported as means and standard deviations (SD). Group comparisons were made using the Chi-square test for categorical variables and the Student’s T-test or Mann–Whitney U test for continuous variables, depending on data distribution. The Spearman correlation coefficient was used to assess associations between continuous variables.
Multivariate logistic regression analysis was conducted to identify independent factors associated with parasomnias in children with ADHD. Variables with a p-value < 0.05 in univariate analysis were included in the multivariate model. Adjusted odds ratios (OR) and 95% confidence intervals (CI) were reported. All analyses were performed using SPSS version 22.0, with statistical significance set at p < 0.05.
Ethical Considerations
The study protocol was approved by the Biomedical Research Ethics Committee of Hanoi Medical University (Approval No. 794/GCN-HĐĐĐNCYSH-ĐHYHN). Informed consent was obtained from all caregivers before participation. The study was conducted in compliance with ethical standards and the Declaration of Helsinki.
RESULTS
The study enrolled 629 children aged 6 to 12 years (mean age: 7.8 ± 1.5 years), newly diagnosed with ADHD according to DSM-5 criteria. Of these, 547 (87.0%) were male and 82 (13.0%) were female. Regarding clinical subtypes, 16.3% were classified as hyperactive subtype, 21.5% as inattentive subtype, and 62.2% as combined subtype. A large proportion of participants presented with comorbidities: 66.9% had at least one, and 28.6% had two or more co-occurring disorders.
Prevalence of Parasomnias in Children with ADHD
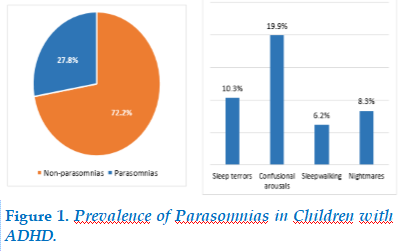
Among the 629 children diagnosed with ADHD, 175 (27.8%) exhibited at least one type of parasomnia. NREM-related parasomnias were the most commonly reported, including sleep terrors, sleepwalking, and confusional arousals. REM-related parasomnias, such as nightmares, were also present but to a lesser extent (Figure 1)
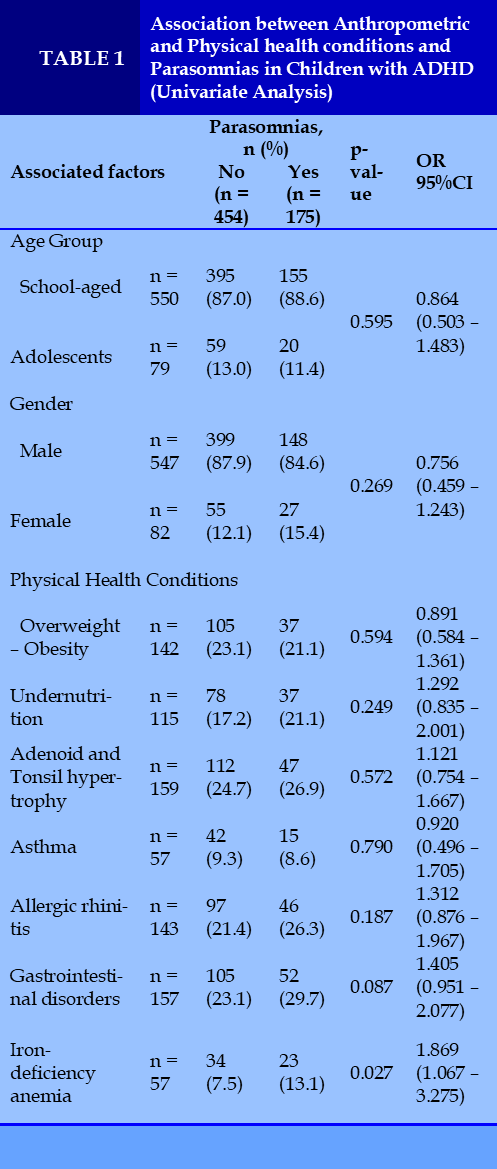
Iron-deficiency anemia was the only factor significantly associated with parasomnias in children with ADHD (p = 0.027, OR = 1.869). Other anthropometric and physical health factors showed no significant associations (Table 1).
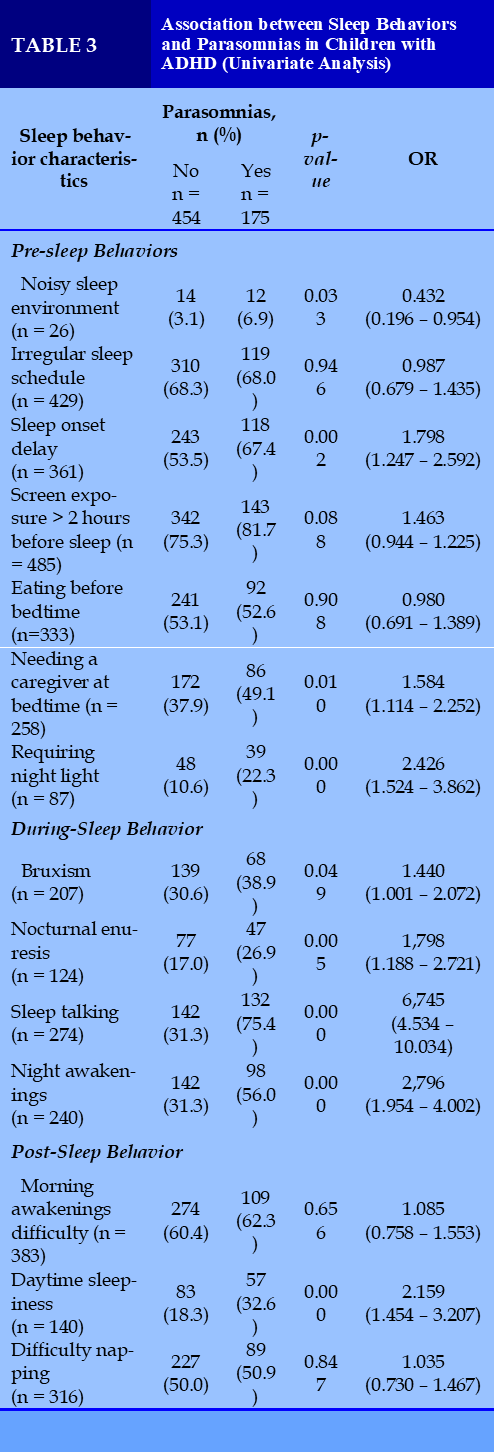
Several pre-sleep and during-sleep behaviors were significantly associated with parasomnias in children with ADHD. Notably, delayed bedtime, need for caregiver presence, sleep talking, and frequent night awakenings showed strong associations. Post-sleep behaviors were mostly not significant, except for daytime sleepiness (Table 3).
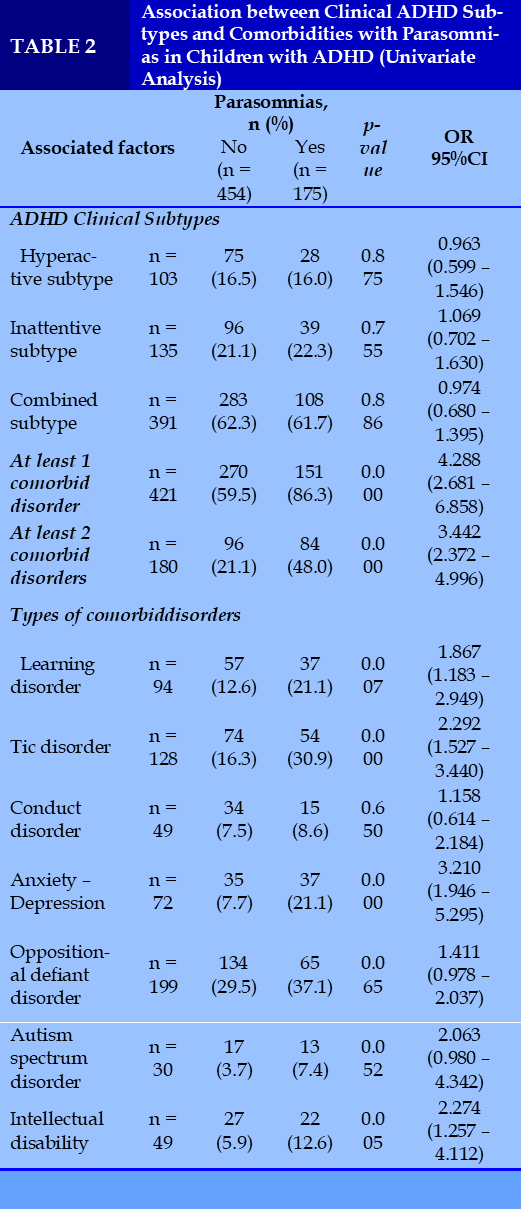
Children with ADHD who had at least one or two comorbid disorders were significantly more likely to experience parasomnias.
Specific comorbidities such as learning disorders, tic disorders, anxiety – depression, and intellectual disability showed strong associations with parasomnias.
In contrast, ADHD clinical subtypes did not show a significant relationship with parasomnias (Table 2).
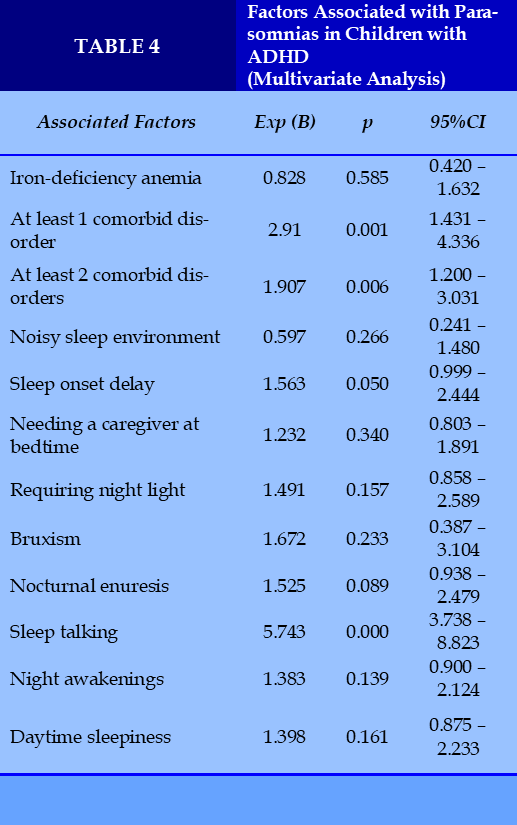
In multivariate analysis, the presence of at least one or two comorbid disorders and sleep talking were independently associated with parasomnias in children with ADHD. Sleep talking showed the strongest association (OR = 5.743, p < 0.001). Other factors such as iron-deficiency anemia, night awakenings, and sleep onset delay were not statistically significant after adjustment (Table 4).
DISCUSSION
This study investigated the prevalence and associated factors of parasomnias in a large cohort of Vietnamese children newly diagnosed with ADHD.
We found that 27.8% of participants experienced at least one type of parasomnia, with NREM-related events such as sleep terrors and confusional arousals being the most common. These findings are consistent with previous literature reporting that children with ADHD are at increased risk of parasomnias and other sleep disturbances. [6,12]
Notably, our results indicate that the presence of comorbid psychiatric disorders is a strong predictor of parasomnias.
Children with at least one comorbid condition had over twice the risk, and those with two or more comorbidities had nearly four times the odds of parasomnias. Specific comorbidities such as tic disorders, anxiety–depression, intellectual disability, and learning disorders were significantly associated with increased parasomnia risk.
These findings align with previous studies suggesting that neurodevelopmental and emotional dysregulation can alter arousal thresholds during sleep and increase susceptibility to parasomnias.[5,9]Among sleep-related behaviors, sleep talking emerged as the strongest independent predictor (OR = 5.743), even after adjusting for other variables. Other behaviors such as night awakenings and delayed bedtime also showed significant associations in univariate analysis, though their effects did not remain statistically significant in the multivariate model. This supports the hypothesis that fragmented sleep and poor sleep hygiene may contribute to instability in sleep stages, facilitating parasomnias in vulnerable children.[7]
Interestingly, iron-deficiency anemia, although associated with parasomnias in univariate analysis, was not significant in the multivariate model. This contrasts with studies suggesting a role of iron in dopamine regulation and arousal mechanisms,13 and warrants further investigation in more targeted cohorts.
Contrary to some expectations, ADHD clinical subtypes were not associated with parasomnias, suggesting that the risk may be more strongly linked to co-occurring conditions and environmental or behavioral factors than to the ADHD presentation itself.
This study has several strengths, including its large sample size, standardized diagnostic criteria (DSM-5 and ICSD-3), and comprehensive assessment of comorbidities and sleep behaviors. However, limitations include its cross-sectional design, which precludes causal inference, and reliance on parent-reported sleep behaviors, which may be subject to recall bias. Objective sleep assessments such as polysomnography and actigraphy were not employed and should be considered in future research. Future studies should adopt longitudinal designs to explore the causal relationship between ADHD and parasomnias, particularly how sleep disturbances evolve over time and their impact on ADHD symptom severity. Additionally, investigating underlying neurobiological mechanisms, including dopaminergic dysfunction and autonomic dysregulation, could provide further insights into the interplay between sleep and ADHD. Finally, clinical trials evaluating behavioral and pharmacological interventions for sleep disturbances in ADHD populations are warranted to develop targeted treatment strategies.
CONCLUSION
This study demonstrates a high prevalence of parasomnias in children with ADHD, with strong associations with comorbid psychiatric disorders and sleep-related behaviors, particularly sleep talking.
These findings emphasize the importance of routine sleep assessments in ADHD management. Future research should focus on longitudinal studies, neurobiological mechanisms, and targeted interventions to better understand and address sleep disturbances in this population.
CONFLICT OF INTEREST
Non.
REFERENCES
| 1. Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942-948. doi:10.1176/ajp.2007.164.6.942 |
| 2. Hodgkins P, Setyawan J, Mitra D, et al. Management of ADHD in children across Europe: patient demographics, physician characteristics and treatment patterns. Eur J Pediatr. 2013;172:895-906. |
| 3. Carter KA, Hathaway NE, Lettieri CF. Common sleep disorders in children. Am Fam Physician. 2014;89(5):368-377. |
| 4. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387-1394. doi:10.1378/chest.14-0970 |
| 5. Ivanenko A, Crabtree VM, Obrien LM, Gozal D. Sleep complaints and psychiatric symptoms in children evaluated at a pediatric mental health clinic. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2006;2(1):42-48. |
| 6. Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry. 2009;48(9):894-908.doi:10.1097/CHI.0b013e3181ac09c9 |
| 7. Yoon SYR, Jain U, Shapiro C. Sleep in attention-deficit/hyperactivity disorder in children and adults: past, present, and future. Sleep Med Rev. 2012;16(4):371-388. doi:10.1016/j.smrv.2011.07.001 |
| 8. Corkum P, Tannock R, Moldofsky H. Sleep disturbances in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1998;37(6):637-646.doi:10.1097/00004583-199806000-00014 |
| 9. Al Lihabi A. A literature review of sleep problems and neurodevelopment disorders. Front Psychiatry. 2023;14:1122344. doi:10.3389/fpsyt.2023.1122344 |
| 10. Sung V, Hiscock H, Sciberras E, Efron D. Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Arch Pediatr Adolesc Med. 2008;162(4):336-342.doi:10.1001/archpedi.162.4.336 |
| 11. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM, 5th Ed. American Psychiatric Publishing, Inc.; 2013:xliv, 947. doi:10.1176/appi.books.9780890425596 |
| 12. Owens JA. The ADHD and sleep conundrum: a review. J Dev Behav Pediatr JDBP. 2005;26(4):312-322. doi:10.1097/00004703-200508000-00011 |
| 13. Konofal E, Lecendreux M, Arnulf I, Mouren MC. Iron deficiency in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med. 2004;158(12):1113-1115.doi:10.1001/archpedi.158.12.1113 |
FIGURES - TABLES
REFERENCES
| 1. Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942-948. doi:10.1176/ajp.2007.164.6.942 |
| 2. Hodgkins P, Setyawan J, Mitra D, et al. Management of ADHD in children across Europe: patient demographics, physician characteristics and treatment patterns. Eur J Pediatr. 2013;172:895-906. |
| 3. Carter KA, Hathaway NE, Lettieri CF. Common sleep disorders in children. Am Fam Physician. 2014;89(5):368-377. |
| 4. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387-1394. doi:10.1378/chest.14-0970 |
| 5. Ivanenko A, Crabtree VM, Obrien LM, Gozal D. Sleep complaints and psychiatric symptoms in children evaluated at a pediatric mental health clinic. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2006;2(1):42-48. |
| 6. Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry. 2009;48(9):894-908.doi:10.1097/CHI.0b013e3181ac09c9 |
| 7. Yoon SYR, Jain U, Shapiro C. Sleep in attention-deficit/hyperactivity disorder in children and adults: past, present, and future. Sleep Med Rev. 2012;16(4):371-388. doi:10.1016/j.smrv.2011.07.001 |
| 8. Corkum P, Tannock R, Moldofsky H. Sleep disturbances in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1998;37(6):637-646.doi:10.1097/00004583-199806000-00014 |
| 9. Al Lihabi A. A literature review of sleep problems and neurodevelopment disorders. Front Psychiatry. 2023;14:1122344. doi:10.3389/fpsyt.2023.1122344 |
| 10. Sung V, Hiscock H, Sciberras E, Efron D. Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Arch Pediatr Adolesc Med. 2008;162(4):336-342.doi:10.1001/archpedi.162.4.336 |
| 11. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM, 5th Ed. American Psychiatric Publishing, Inc.; 2013:xliv, 947. doi:10.1176/appi.books.9780890425596 |
| 12. Owens JA. The ADHD and sleep conundrum: a review. J Dev Behav Pediatr JDBP. 2005;26(4):312-322. doi:10.1097/00004703-200508000-00011 |
| 13. Konofal E, Lecendreux M, Arnulf I, Mouren MC. Iron deficiency in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med. 2004;158(12):1113-1115.doi:10.1001/archpedi.158.12.1113 |
ARTICLE INFO DOI: 10.12699/jfvpulm.16.49.2025.1
Conflict of Interest
Non
Date of manuscript receiving
10/03/2025
Date of publication after correction
18/06/2025
Article citation
Mai Nguyen-Thi-Phuong, Mai Nguyen-Thi-Thanh, Sy Duong-Quy. Association between parasomnias and children with attention deficit hyperactivity disorder: A cross-sectional study in Vietnam. J Func Vent Pulm 2025;49(16):1-6