
 English
English
 French
French
Sleep medicine and sport: facts, challenges and solutions for Vienam
Médecine du sommeil et sport: faits, défis et solutions pour le Vienam
Sy Duong-Quy1,2,3,4, Nghia Ly-Dai5, Bao Le-Khac1,6, Vinh Nguyen-Nhu1,6, Khue Bui-Diem1,6 , Thu Nguyen-Ngoc-Phuong1,7, Diep Nguyen-Thi-Hong1, Tinh Vo-Van1,7, Anh Nguyen-Tuan1,2, Tu Tran-Thi-Cam1, Tram Tang-Thi-Thao1,2, Huong T.X Hoang1,8, Toi Nguyen-Van1,2, Thai Nguyen-Duy1,3,9, Ngoc Luu-Bich10, Dung Nguyen-Thi-Thu1,11, Long Nguyen-Viet12, Chong Cao-Van13
1Vietnam Society of Sleep Medicine. Lam Dong, Vietnam
2Lam Dong Medical College. Lam Dong, Vietnam
3Department of Sleep Medicine. University of Medicine and Pharmacy. Hanoi National University. Hanoi, Vietnam
4Penn State Medical College. PA, USA
5Training and Sport Competition Center of Ho Chi Minh City, Vietnam
6University of Medicine and Pharmacy at Ho Chi Minh city. Ho Chi Minh, Vietnam
7Pham Ngoc Thach University. Ho Chi Minh, Vietnam
8Phenikaa University. Hanoi, Vietnam
9Ministry of Health. Hanoi, Vietnam
10National Council of Education and Human Resources of Vietnam. Hanoi, Vietnam
11Thai Binh Medical College Hospital. Thai Binh Medical College. Hung Yen, Vietnam
12Committee of Propaganda and Popular Promotion of Ho Chi Minh City, Vietnam
13Department of Culture and Sport of Ho Chi Minh City, Vietnam
Corresponding author: Sy Duong-Quy. Sleep Medicine Research Center. Vietnam Society of Sleep Medicine. Lam Dong, Viet Nam.
Mail: sduongquy.jfvp@gmail.com
ABSTRACT
Sleep medicine is a vital component of elite athlete health and performance. Research shows that sleep duration, quality, and circadian alignment are essential for recovery, cognitive and emotional function, injury prevention, and competitive success. Poor sleep or untreated sleep disorders negatively affect training capacity, decision-making, reaction time, and increase injury risk. The paper reviews the importance of sleep health in elite sports, particularly highlighting challenges in integrating sleep medicine into athlete care systems in developing and transitional countries. Good sleep supports neuromuscular recovery, hormonal balance, immune function, and learning, while chronic sleep deprivation, circadian disruption, and sleep disorders impair performance and raise injury rates. It also proposes evidence-based strategies to improve sleep, including sleep hygiene, behavioral interventions, optimized training schedules, travel adaptation, and policy-level solutions such as systematic sleep assessment, staff training, use of AI and wearable technologies, and the development of specialized sleep medicine centers. Overall, the paper emphasizes that integrating sleep medicine into high-performance sport systems is essential for sustainable performance and long-term athlete development.
KEYWORDS: Sleep medicine; Elite athletes; Performance; Injury prevention.
RÉSUMÉ
La médecine du sommeil est un élément essentiel de la santé et de la performance des athlètes d’élite. Les recherches montrent que la durée, la qualité du sommeil et l’alignement circadien sont indispensables à la récupération, aux fonctions cognitives et émotionnelles, à la prévention des blessures et à la réussite en compétition. Un sommeil insuffisant ou des troubles du sommeil non traités affectent négativement la capacité d’entraînement, la prise de décision et le temps de réaction, tout en augmentant le risque de blessures. Cet article examine l’importance de la santé du sommeil dans le sport de haut niveau, en soulignant particulièrement les défis liés à l’intégration de la médecine du sommeil dans les systèmes de prise en charge des athlètes, notamment dans les pays en développement et en transition. Un bon sommeil favorise la récupération neuromusculaire, l’équilibre hormonal, la fonction immunitaire et l’apprentissage, tandis que la privation chronique de sommeil, les perturbations du rythme circadien et les troubles du sommeil altèrent la performance et augmentent l’incidence des blessures. L’article propose également des stratégies fondées sur des preuves pour améliorer le sommeil, incluant l’hygiène du sommeil, les interventions comportementales, l’optimisation des horaires d’entraînement, l’adaptation aux déplacements, ainsi que des solutions au niveau des politiques, telles que l’évaluation systématique du sommeil, la formation du personnel, l’utilisation de l’intelligence artificielle et des technologies portables, et le développement de centres spécialisés en médecine du sommeil. Dans l’ensemble, l’article souligne que l’intégration de la médecine du sommeil dans les systèmes sportifs de haut niveau est essentielle pour une performance durable et le développement à long terme des athlètes.
MOTS CLÉS: Médecine du sommeil; Athlètes de haut niveau; Performance; Prévention des blessures.
1. Background of The Role of Sleep Medicine in High-Performance Sport
Sleep medicine plays a critically important role in human life, as more than one-third of an individual’s lifetime is spent sleeping. Adequate and high-quality sleep contributes to increased longevity, reduced morbidity, and enhancement of immune system function, thereby protecting the body against disease. Good-quality sleep supports musculoskeletal health, improves cognitive clarity and alertness upon awakening, and enhances learning capacity, work productivity, and training efficiency. Consequently, sleep quality directly influences athletic performance and competitive success [1-6].
For athletes, particularly those engaged in high-performance sport, sleep represents a vital period during which multiple physiological systems recover following prolonged and intensive physical exertion. Sleep provides the necessary biological conditions for tissue repair, neuromuscular recovery, metabolic regulation, and hormonal balance, thereby preparing the athlete for optimal physical condition and readiness for subsequent training sessions or high-level competition [1-3]. For this reason, both athletes and coaches must be equipped with fundamental knowledge of sleep medicine, and sports medicine teams should include healthcare professionals trained in sleep science as part of comprehensive athlete care. Despite decades of attention to sleep optimization in developed countries with advanced sports medicine systems, where elite athletes are routinely included in sleep monitoring programs, high-performance surveillance systems, injury prevention strategies, and long-term athlete development pathways, sleep medicine remains under-recognized in many developing and transitional countries. In Vietnam, in particular, the integration of sleep medicine into high-performance sport development has not yet received adequate attention or systematic implementation.
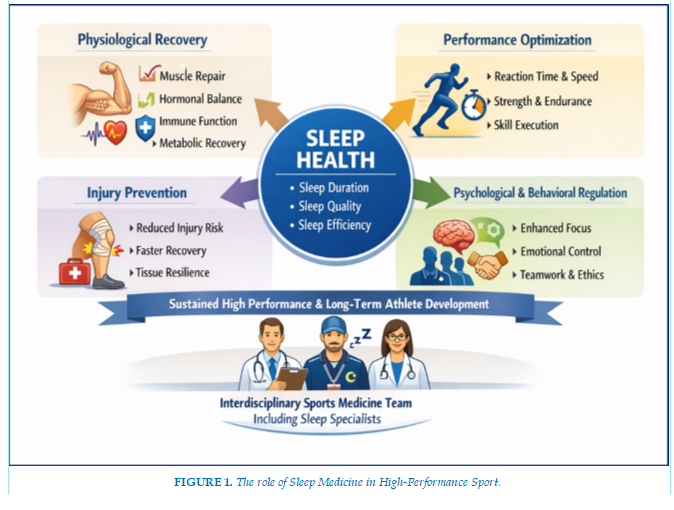
Scientific evidence published has consistently demonstrated a strong association between sleep health and elite athletic performance. These studies confirm that maintaining good sleep quality and optimal sleep efficiency is essential for achieving, sustaining, and improving high-level performance [1-3]. Furthermore, adequate sleep reduces the risk of training- and competition-related injuries and positively influences athletes’ behavioral regulation, emotional control, and ethical conduct. These benefits are especially evident in sports characterized by high physical contact and team interaction, such as volleyball, football (soccer), rowing, relay running, and other team-based or combative disciplines. (Figure 1)
2. The Role of Sleep Health in High-Performance Sport
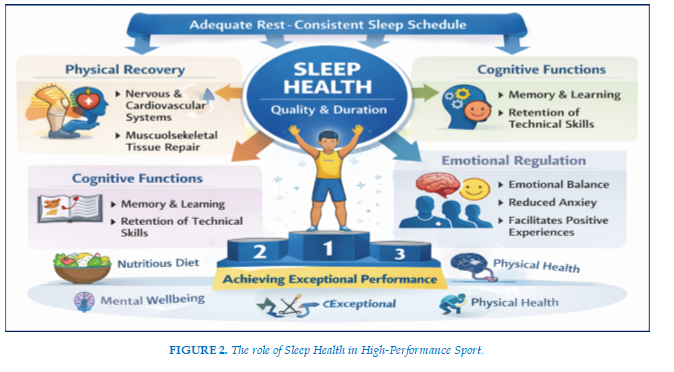
To achieve optimal training and competitive performance, elite athletes must be comprehensively prepared in terms of physical health, mental well-being, and emotional balance. Sleep quality and sleep duration play a particularly important role in the physical development of young athletes, adolescent athletes, and even athletes over the age of 18. Therefore, in addition to maintaining regular training programs prescribed by coaching staff, elite athletes must ensure a scientifically balanced diet under the guidance of sports nutrition specialists and, most importantly, allocate sufficient time for rest, recovery, and regular, adequate sleep [4].
When sleep duration is insufficient or misaligned with the athlete’s biological rhythm, such as in cases of circadian disruption and jet lag caused by training or competing in countries located in different time zones, competitive performance at both the individual and team levels may be adversely affected if appropriate countermeasures are not implemented [7-9].
High-quality sleep enables the nervous system, cardiovascular–respiratory system, musculoskeletal system, and metabolic–excretory systems, particularly in elite athletes, to rest, recover, and function in accordance with normal circadian rhythms following days of high-intensity training or competition. Sleep facilitates cellular regeneration, repair of healthy tissues, and healing of musculoskeletal micro-injuries accumulated during intense physical activity [2,3]. In addition, good sleep quality enhances memory consolidation, assimilation of coaching instructions, and the acquisition of refined and complex technical skills.
Moreover, good sleep health, reflected by high-quality sleep, supports the regulation and stabilization of mental and emotional states, helping to prevent anxiety, stress, and depressive symptoms. Sleep medicine research has demonstrated that restorative sleep enables athletes to retain positive emotions and memories associated with training and competition while attenuating negative emotional experiences. Consequently, good sleep health facilitates the learning of new skills, enhances creative thinking and empathy, promotes positive memory formation, and ultimately contributes to improved high-performance outcomes in competition [2].
Conversely, poor sleep health—characterized by insufficient sleep duration or low sleep quality—impairs the sustainable development of learning capacity, memory formation, and accurate skill execution, while significantly increasing the risk of injury during training and competition. Chronic sleep deprivation, in particular, leads to cognitive decline and may exert detrimental effects on athletes when they are placed in situations requiring high levels of concentration, rapid reflexes, and advanced decision-making, such as critical tactical decisions and precise execution of complex technical actions during competition [10,11].
Furthermore, high-quality sleep plays a vital role in maintaining mental and psychophysiological health in athletes in general and elite athletes in particular. Restorative sleep promotes positive thoughts and emotions, helps prevent unnecessary worry and distress during daily training and competition, and reduces impulsivity and emotional instability in high-contact and confrontational sports, where competitive situations frequently involve physical collisions and heightened emotional demands. (Figure 2)
3. The Role of Sleep Health in High-Performance Training and Competition
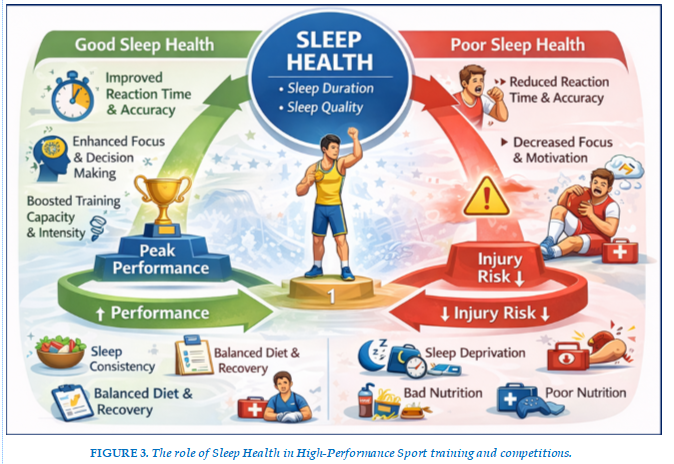
Sleep medicine research has demonstrated that increasing sleep duration and improving sleep quality in athletes, particularly elite athletes, are associated with significant improvements in athletic performance and competitive outcomes [5,6]. In addition, good sleep health can markedly reduce the risk of injury, thereby indirectly enhancing performance by allowing athletes to maintain higher training frequency and intensity and to participate more consistently in competition. Numerous studies have shown that extending sleep duration enables athletes to compete at their optimal level and achieve peak performance, whereas poor sleep quality or sleep deprivation impairs concentration, slows reaction time and accuracy, and reduces the ability to make sound, strategic decisions during competitive situations [2,5].
Therefore, it is a matter of concern when elite athletes are not adequately educated or equipped with knowledge of good sleep health practices, fail to obtain sufficient sleep, or neglect basic sleep hygiene principles. Sleep deprivation reduces competitive motivation due to persistent fatigue, excessive daytime sleepiness, and increased muscle stiffness, thereby limiting athletes’ capacity to meet the demanding requirements of high-performance sport. Insufficient sleep also accelerates physical exhaustion, particularly when athletes compete under unfavorable environmental conditions such as extreme heat, cold, or high altitude [10-11]. Moreover, sleep deprivation diminishes the ability to execute complex and highly precise technical movements required in sports such as gymnastics, martial arts, and shooting, compared with conditions of adequate and restorative sleep. In high-contact and combative elite sports, athletes who are sleep-deprived or experience poor sleep quality demonstrate slower and less accurate reactions and impaired situational responses during competition.
The increased risk of injury during training and competition among elite athletes with sleep disturbances, including snoring and obstructive sleep apnea, insomnia, parasomnias, or chronic sleep deprivation has been well documented in numerous published studies. Research findings indicate that chronic sleep deficiency significantly increases injury incidence among elite athletes during both training and competition. Insufficient sleep duration or poor sleep quality exacerbates musculoskeletal strain and trauma, increasing vulnerability to injury. Indeed, the risk and prevalence of injuries in elite sport are closely associated with excessive training loads combined with inadequate sleep duration or suboptimal sleep quality. Both acute and chronic sleep deprivation impair accuracy and attentional focus during the execution of complex technical skills, thereby substantially increasing the likelihood of injury in both training and competitive settings [1-3]. (Figure 3)
4. Methods to Help Elite Athletes Maintain Good Sleep Health
4.1. Adherence to Sleep Hygiene Practices
Athletes should be provided with basic knowledge and be required to strictly adhere to a scientific and structured sleep hygiene regimen that is appropriate for their training and competition conditions. Core components of sleep hygiene include avoiding alcohol and coffee at least six hours before bedtime, as these beverages—especially those containing caffeine—can disrupt sleep continuity, increase nocturnal awakenings, and prolong sleep onset latency. Caffeine, in particular, enhances alertness and delays the transition into both light and deep sleep stages. Athletes should also avoid smoking before bedtime and are strongly encouraged to cease tobacco use altogether.
Athletes should refrain from using tablets, smartphones, or playing electronic games after 20:00, as exposure to blue light emitted by these devices directly stimulates the retina and suppresses melatonin secretion [12]. Melatonin, a hormone secreted by the pineal gland, plays a critical role in promoting sleep onset and deep sleep and also contributes to immune system regulation. Prolonged evening exposure to blue light disrupts circadian rhythms and promotes delayed sleep–wake phase patterns (late sleep onset and late awakening), leading to non-restorative sleep and a persistent sensation of sleep deprivation in elite athletes.
4.2. Techniques to Improve Sleep Quality
To achieve deep and restorative sleep, elite athletes should receive guidance on sleep-enhancing techniques, such as establishing a relaxing pre-sleep routine. Activities including reading, taking a warm bath, practicing controlled breathing exercises, yoga, or meditation are effective strategies for facilitating sleep onset following days of high-intensity training or competition. When athletes experience prolonged sleep onset latency, they should avoid remaining in bed while awake for extended periods. Instead, if unable to fall asleep within 20–30 minutes, they should leave the bed and engage in quiet, low-stimulation activities in another space until drowsiness develops, then return to bed. Each athlete should also optimize their sleep environment by using dim lighting, maintaining a cool and quiet bedroom, wearing appropriate sleepwear, and using socks for warmth in colder conditions.
4.3. Maintaining a Rational and Scientific Training and Competition Schedule
To preserve good sleep health and ensure high-quality sleep, elite athletes should avoid excessive training loads that lead to physical exhaustion, excessive muscle strain, and microtrauma, which may cause musculoskeletal pain and interfere with sleep initiation and depth. Except for unavoidable competition schedules, athletes and coaching staff should minimize training sessions or competitions scheduled very early in the morning or late at night, as these can disrupt circadian rhythms and physiological sleep patterns. In tropical climates, a short daytime nap of approximately 20 minutes can be beneficial for athletes, improving afternoon training and competition performance and reducing fatigue following morning training sessions. Additionally, elite athletes should minimize excessive psychological stressors during both training and rest periods, as mental stress negatively affects sleep quality and recovery.
4.4. Early Adaptation to Jet Lag
Jet lag is a common external factor that disrupts circadian rhythms in both athletes and coaching staff when training or competing internationally [9,11]. This condition is a major contributor to persistent fatigue following long-distance travel and can significantly impair competitive performance, particularly during international tournaments.
Therefore, prior to international travel, coaching staff and athletes should consider the time zone difference between the departure and destination countries and gradually adjust daily routines—including meal timing, training schedules, and sleep–wake patterns—to align with the destination time zone. Athletes should adjust their watches to the destination time immediately upon boarding the aircraft. During long-haul flights, maintaining activity, meals, and sleep according to the destination’s biological time helps facilitate rapid adaptation and enables athletes and staff to integrate into the local schedule immediately upon arrival. (Figure 4)
5. Policy Solutions for the Development of Sleep Medicine in Comprehensive Health Care for Elite Athletes
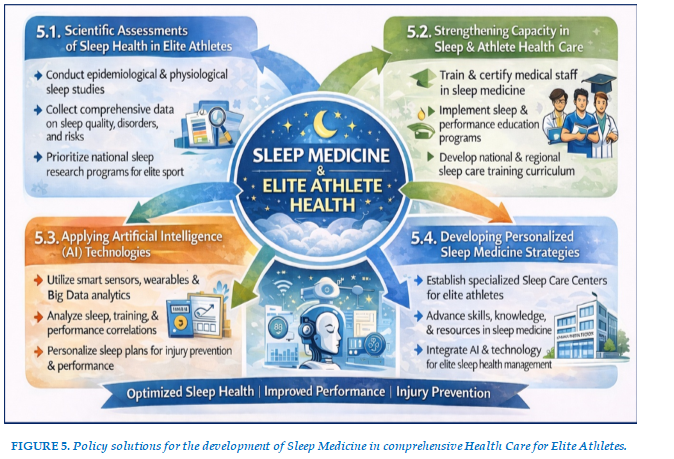
5.1. Conducting Objective, Comprehensive Scientific Assessments of Sleep Health Status in Elite Athletes
Objective and systematic scientific assessments provide the essential evidence base for collecting data on sleep disorders, sleep deprivation, and poor sleep hygiene resulting from failure to avoid behaviors harmful to sleep quality [13,14]. Epidemiological studies indicate that more than 8.5% of Vietnamese adults aged over 18 years suffer from sleep-disordered breathing, particularly obstructive sleep apnea, which causes excessive daytime sleepiness and fatigue, while more than 25% of this age group and younger populations experience insufficient sleep due to various factors [15-19].
Therefore, governmental authorities responsible for sport administration, healthcare, and science and technology should prioritize research programs aimed at assessing the health status of athletes—especially elite athletes—as a core component of national sports development strategies [13].
5.2. Strengthening Capacity for Comprehensive Health Care and Sleep Health Management Among Medical Staff Serving Elite Athletes
This represents an urgent requirement in developing a national strategy for elite sport under the principle that “sleep health is the foundation of high performance.” Currently, medical personnel at local levels and within sports institutions, particularly in elite sport, often lack basic training in sleep medicine and may not fully recognize the critical role of sleep health in training quality, competition performance, and elite achievement [20].
Accordingly, relevant governing bodies should develop structured training and certification programs in sleep medicine for healthcare professionals working with elite athletes. These programs may be delivered through the Vietnam Sleep Medicine Society, as well as national, regional, and international specialized workshops and continuing medical education initiatives [20,21].
5.3. Application of Artificial Intelligence Technologies to Analyze Relationships Between Sleep Health Parameters, Training Load, and Performance Outcomes
Current practice indicates that despite significant socioeconomic development and widespread adoption of advanced technologies in areas such as digital communication, public services, and smart city initiatives, the application of artificial intelligence (AI) in healthcare—and specifically in sleep health management based on machine learning, deep learning, and big data analytics—remains underdeveloped compared with other countries in the region [12,18].
The implementation of AI-based strategies for sleep health management in elite athletes has become increasingly feasible due to the availability of smart devices capable of continuous, non-invasive data collection. These include wearable devices, smart rings, smart pillows, and smart beds, which utilize actigraphy, acoustic signals, electromagnetic sensing, functional electroencephalography proxies, and circadian rhythm biomarkers [12,19].
Through deep learning algorithms, AI systems can personalize sleep health recommendations according to sport-specific demands, age, training intensity, nutritional patterns, and overall physiological status. These systems can support individualized training planning, optimize recovery strategies, and generate evidence-based recommendations to reduce injury risk during elite training and competition.
5.4. Developing Personalized Sleep Medicine Strategies for Elite Athletes and Enhancing Skills, Knowledge, and Resources for Healthcare Providers
This is a critical requirement for advancing sleep medicine with the goal of “good sleep health for injury prevention and performance enhancement.” In Vietnam, it is necessary to establish specialized units dedicated to sleep health care for elite athletes through the development of “Sleep Care Centers” serving both the general population and sport-specific needs [16]. These centers should be equipped with advanced diagnostic and monitoring technologies to conduct periodic sleep health assessments, design individualized consultation programs, and implement tailored interventions to maintain athletes’ health at optimal levels and support peak competitive performance [16]. Such initiatives would also provide the foundation for establishing an “Institute of Applied Sleep Medicine in High-Performance Sport,” tasked with education and training, scientific research, technology transfer, and international collaboration. This institute would integrate advances in sleep medicine, sports medicine, comorbid medical diseases and artificial intelligence to support the holistic development of elite athletes—including physical performance, emotional intelligence, technical competence, and sports ethics—through personalized programs in nutrition, training, recovery, and sport-specific skills, contributing to elite sport development in major Vietnamese cities such as Ho Chi Minh City, Hanoi, and at the national level [4,16,20,21].(Figure 5)
6. Conclusion
Sleep medicine plays a critically important role in ensuring effective training capacity and achieving optimal competitive outcomes in elite athletes. In addition to health issues addressed by sports medicine, the implementation of appropriate nutritional strategies, the consistent application of progressive, modern, and scientific training methods, together with good sleep health, enables elite athletes to fully develop their potential and achieve peak performance. Integrating sleep medicine with sports medicine, personalized medicine, and the application of artificial intelligence technologies in training and competition—combined with the unique physiological and psychological characteristics of elite athletes—will enable Vietnam’s high-performance sports system to achieve substantial and sustainable advancement.
Therefore, national sports academies should incorporate fundamental sleep medicine content into their training curricula. Training and coaching institutions should prioritize the maintenance of optimal sleep health for elite athletes alongside evidence-based nutrition and scientifically designed training programs to ensure the highest competitive achievements. Local authorities should take the lead in developing strategies under the principle of “Good Sleep Health for Elite Athletes,” in coordination with national professional bodies such as the Ministry of Health and the Vietnam Sleep Medicine Society, to establish “Institutes of Sleep Medicine and High-Performance Sports Medicine.” This represents a strategic breakthrough for the current period and a forward-looking vision toward 2030, strengthening the integration of sports medicine and sleep medicine, incorporating periodic sleep quality assessments into advanced scientific training programs. Such an approach is essential, because “good sleep is a fundamental prerequisite for high performance.”
REFERENCES
| 1. Fullagar HHK, Skorski S, Duffield R, Hammes D, Coutts AJ, Meyer T. Sleep and athletic performance: The effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015;45(2):161–186. |
| 2. Mah CD, Mah KE, Kezirian EJ, Dement WC. |
| The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep. 2011;34(7):943–950. |
| 3. Watson AM. Sleep and athletic performance. Curr Sports Med Rep. 2017;16(6):413–418. |
| 4. Halson SL, Juliff LE. Sleep, sport, and the brain. Prog Brain Res. 2017;234:13–31. |
| 5. Halson SL. Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med. 2014;44(Suppl 1):S13–S23. |
| 6. Buxton OM, Chang AM, Spilsbury JC, Bos T, Emsellem H, Knutson KL. Sleep in the modern family: Protective family routines for child and adolescent sleep. Sleep Health. 2015;1(1):15–27. |
| 7. Chang AM, Aeschbach D, Duffy JF, Czeisler CA. |
| Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci U S A. 2015;112(4):1232–1237. |
| 8. Reilly T, Waterhouse J, Edwards B. Jet lag and air travel: Implications for performance. Clin Sports Med. 2005;24(2):367–380. |
| 9. Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: Dose–response effects on neurobehavioral functions and sleep physiology. Sleep. 2003;26(2):117–126. |
| 10. Waterhouse J, Reilly T, Atkinson G, Edwards B. Jet lag: Trends and coping strategies. Lancet. 2007;369(9567):1117–1129. |
| 11. Krause AJ, Simon EB, Mander BA, et al. The sleep-deprived human brain. Nat Rev Neurosci. 2017;18(7):404–418. |
| 12. Peake JM, Kerr G, Sullivan JP. A critical review of consumer wearables, mobile applications, and equipment for providing biofeedback, monitoring stress, and sleep in physically active populations. Front Physiol. 2018;9:743. |
| 13. Buysse DJ. Sleep health: Can we define it? Does it matter? Sleep. 2014;37(1):9–17. |
| 14. Walsh NP, Halson SL, Sargent C, et al. Sleep and the athlete: Narrative review and 2021 expert consensus recommendations. Br J Sports Med. 2021;55(7):356–368. |
| 15. Duong-Quy S, Dang Thi Mai K, Tran Van N, et al. [Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam]. Rev Mal Respir. 2018;35(1):14–24. |
| 16. Duong-Quy S, Nguyen-Huu H, Hoang-Chau-Bao D, et al. Personalized medicine and obstructive sleep apnea. J Pers Med. 2022;12(12):2034. |
| 17. Duong-Quy S, Hoc TV, Nguyen-Duy T, Tang-Thi-Thao T, Nguyen-Van T, Huynh-Anh T, Mai-Xuan T, Tran-Quang P, Nguyen-Ba V, Nguyen-Trong B, Nguyen-Ngoc-Phuong T, Doan-Ngoc H, Vu-Van G, Nguyen-Viet N, Soyez F, Martin F, Penzel T, Kushida C, Craig T. Hyperbaric Oxygen Therapy and Its Physio-Mechanical Effects on Sleep Breathing Disorder: A Systematic Review. Pulm Ther. 2025 Nov 28. |
| 18. Duong-Quy S, Nguyen-Duy T, Hoc TV, Nguyen-Thi-Hong L, Tang-Thi-Thao T, Bui-Diem K, Nguyen-Thi-Hong D, Nguyen-Trong B, Nguyen-Tuan A, Nguyen-Huu H, Vu-Tran-Thien Q, Nguyen-Van T, Mai-Xuan T, Nguyen-Ba V, Vo-Pham-Minh-Thu T, Pham-Van T, Pham-Van L, Vu-Van G, Le-Khac B, Nguyen-Thi-Thu D, Luong-Ngoc K, Luu-Bich N, Tran-Phan-Chung T, Le-Thi-Minh H, Nguyen-Nhu V, Nguyen-Viet N, Craig T, Soyez F, Martin F, Penzel T. Self-Administered Home Sleep Testing Model in Screening of OSA in Healthcare Workers-Sohew Study: A National Multicenter Study in Vietnam. Pulm Ther. 2025 Dec;11(4):625-643. |
| 19. Bui-Diem K, Van Tho N, Nguyen-Binh T, Doan-Truc Q, Trinh HKT, Truong DDK, Le KM, Phung Khanh L, Duong-Quy S. Melatonin and Cortisol Concentration Before and After CPAP Treatment of Obstructive Sleep Apnea. Nat Sci Sleep. 2025 Sep 13;17:2201-2212. |
| 20. Duong-Quy S. Letter From the Vietnam Respiratory Society-Vietnam's Respiratory Medicine in Transition: From Clinical Advances to National Healthcare Policy. Respirology. 2025 Dec 15. |
| 21. Duong-Quy S, Huynh-Anh T, Vo-Pham-Minh T, Tran-Thanh-Duy L, Le-Thi-Hong D, Bui-Viet T, Nguyen-Quang T, Tang-Thi-Thao T, Nguyen-Tuan A, Nguyen-Van T, Hoc TV, Nguyen-Ngoc-Phuong T, Vu-Tran-Thien Q, Bui-Diem K, Nguyen-Trong B, Nguyen-Duy T, Nguyen-Thi-Thu D, Tran-Phan-Chung T, Le-Thi-Minh H, Pham-Van L, Vu-Van G, Nguyen-Nhu V, Le-Khac B, Nguyen-Viet N, Martin F, Penzel T, Kushida C, Craig T. Management of Patients with Asthma, COPD, and OSA in Outpatient Unit: ACOSOU-Global Perspectives and Challenges. Pulm Ther. 2026 Jan 20. |
FIGURES - TABLES

REFERENCES
| 1. Fullagar HHK, Skorski S, Duffield R, Hammes D, Coutts AJ, Meyer T. Sleep and athletic performance: The effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015;45(2):161–186. |
| 2. Mah CD, Mah KE, Kezirian EJ, Dement WC. |
| The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep. 2011;34(7):943–950. |
| 3. Watson AM. Sleep and athletic performance. Curr Sports Med Rep. 2017;16(6):413–418. |
| 4. Halson SL, Juliff LE. Sleep, sport, and the brain. Prog Brain Res. 2017;234:13–31. |
| 5. Halson SL. Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med. 2014;44(Suppl 1):S13–S23. |
| 6. Buxton OM, Chang AM, Spilsbury JC, Bos T, Emsellem H, Knutson KL. Sleep in the modern family: Protective family routines for child and adolescent sleep. Sleep Health. 2015;1(1):15–27. |
| 7. Chang AM, Aeschbach D, Duffy JF, Czeisler CA. |
| Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci U S A. 2015;112(4):1232–1237. |
| 8. Reilly T, Waterhouse J, Edwards B. Jet lag and air travel: Implications for performance. Clin Sports Med. 2005;24(2):367–380. |
| 9. Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: Dose–response effects on neurobehavioral functions and sleep physiology. Sleep. 2003;26(2):117–126. |
| 10. Waterhouse J, Reilly T, Atkinson G, Edwards B. Jet lag: Trends and coping strategies. Lancet. 2007;369(9567):1117–1129. |
| 11. Krause AJ, Simon EB, Mander BA, et al. The sleep-deprived human brain. Nat Rev Neurosci. 2017;18(7):404–418. |
| 12. Peake JM, Kerr G, Sullivan JP. A critical review of consumer wearables, mobile applications, and equipment for providing biofeedback, monitoring stress, and sleep in physically active populations. Front Physiol. 2018;9:743. |
| 13. Buysse DJ. Sleep health: Can we define it? Does it matter? Sleep. 2014;37(1):9–17. |
| 14. Walsh NP, Halson SL, Sargent C, et al. Sleep and the athlete: Narrative review and 2021 expert consensus recommendations. Br J Sports Med. 2021;55(7):356–368. |
| 15. Duong-Quy S, Dang Thi Mai K, Tran Van N, et al. [Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam]. Rev Mal Respir. 2018;35(1):14–24. |
| 16. Duong-Quy S, Nguyen-Huu H, Hoang-Chau-Bao D, et al. Personalized medicine and obstructive sleep apnea. J Pers Med. 2022;12(12):2034. |
| 17. Duong-Quy S, Hoc TV, Nguyen-Duy T, Tang-Thi-Thao T, Nguyen-Van T, Huynh-Anh T, Mai-Xuan T, Tran-Quang P, Nguyen-Ba V, Nguyen-Trong B, Nguyen-Ngoc-Phuong T, Doan-Ngoc H, Vu-Van G, Nguyen-Viet N, Soyez F, Martin F, Penzel T, Kushida C, Craig T. Hyperbaric Oxygen Therapy and Its Physio-Mechanical Effects on Sleep Breathing Disorder: A Systematic Review. Pulm Ther. 2025 Nov 28. |
| 18. Duong-Quy S, Nguyen-Duy T, Hoc TV, Nguyen-Thi-Hong L, Tang-Thi-Thao T, Bui-Diem K, Nguyen-Thi-Hong D, Nguyen-Trong B, Nguyen-Tuan A, Nguyen-Huu H, Vu-Tran-Thien Q, Nguyen-Van T, Mai-Xuan T, Nguyen-Ba V, Vo-Pham-Minh-Thu T, Pham-Van T, Pham-Van L, Vu-Van G, Le-Khac B, Nguyen-Thi-Thu D, Luong-Ngoc K, Luu-Bich N, Tran-Phan-Chung T, Le-Thi-Minh H, Nguyen-Nhu V, Nguyen-Viet N, Craig T, Soyez F, Martin F, Penzel T. Self-Administered Home Sleep Testing Model in Screening of OSA in Healthcare Workers-Sohew Study: A National Multicenter Study in Vietnam. Pulm Ther. 2025 Dec;11(4):625-643. |
| 19. Bui-Diem K, Van Tho N, Nguyen-Binh T, Doan-Truc Q, Trinh HKT, Truong DDK, Le KM, Phung Khanh L, Duong-Quy S. Melatonin and Cortisol Concentration Before and After CPAP Treatment of Obstructive Sleep Apnea. Nat Sci Sleep. 2025 Sep 13;17:2201-2212. |
| 20. Duong-Quy S. Letter From the Vietnam Respiratory Society-Vietnam's Respiratory Medicine in Transition: From Clinical Advances to National Healthcare Policy. Respirology. 2025 Dec 15. |
| 21. Duong-Quy S, Huynh-Anh T, Vo-Pham-Minh T, Tran-Thanh-Duy L, Le-Thi-Hong D, Bui-Viet T, Nguyen-Quang T, Tang-Thi-Thao T, Nguyen-Tuan A, Nguyen-Van T, Hoc TV, Nguyen-Ngoc-Phuong T, Vu-Tran-Thien Q, Bui-Diem K, Nguyen-Trong B, Nguyen-Duy T, Nguyen-Thi-Thu D, Tran-Phan-Chung T, Le-Thi-Minh H, Pham-Van L, Vu-Van G, Nguyen-Nhu V, Le-Khac B, Nguyen-Viet N, Martin F, Penzel T, Kushida C, Craig T. Management of Patients with Asthma, COPD, and OSA in Outpatient Unit: ACOSOU-Global Perspectives and Challenges. Pulm Ther. 2026 Jan 20. |
ARTICLE INFO DOI: 10.12699/jfvpulm.17.52.2026.01
Conflict of Interest
Non
Date of manuscript receiving
10/11/2025
Date of publication after correction
02/02/2026
Article citation
Sy Duong-Quy, Nghia Ly-Dai, Bao Le-Khac, Vinh Nguyen-Nhu, Khue Bui-Diem , Thu Nguyen-Ngoc-Phuong, Diep Nguyen-Thi-Hong, Tinh Vo-Van, Anh Nguyen-Tuan, Tu Tran-Thi-Cam, Tram Tang-Thi-Thao, Huong T.X Hoang, Toi Nguyen-Van, Thai Nguyen-Duy, Ngoc Luu-Bich, Dung Nguyen-Thi-Thu, Long Nguyen-Viet, Chong Cao-Van. Sleep medicine and sport: facts, challenges and solutions for Vienam. J Fran Vent PulmS 2026;52(17):1-8